Subdural hemorrhage is a life-threatening condition that occurs when blood accumulates between the brain and its protective covering. This medical emergency requires immediate recognition and treatment to prevent severe neurological complications or death. Medical professionals, students, and healthcare providers must understand the different types, diagnostic methods, and key differences from similar conditions.
This comprehensive guide will explore the anatomy of subdural hemorrhage, examine CT imaging findings, compare it with other intracranial bleeding types, and provide essential information for proper diagnosis and management. Whether you’re studying for medical exams or treating patients, this article offers crucial insights into one of neurosurgery’s most critical conditions.
What is Subdural Hemorrhage?
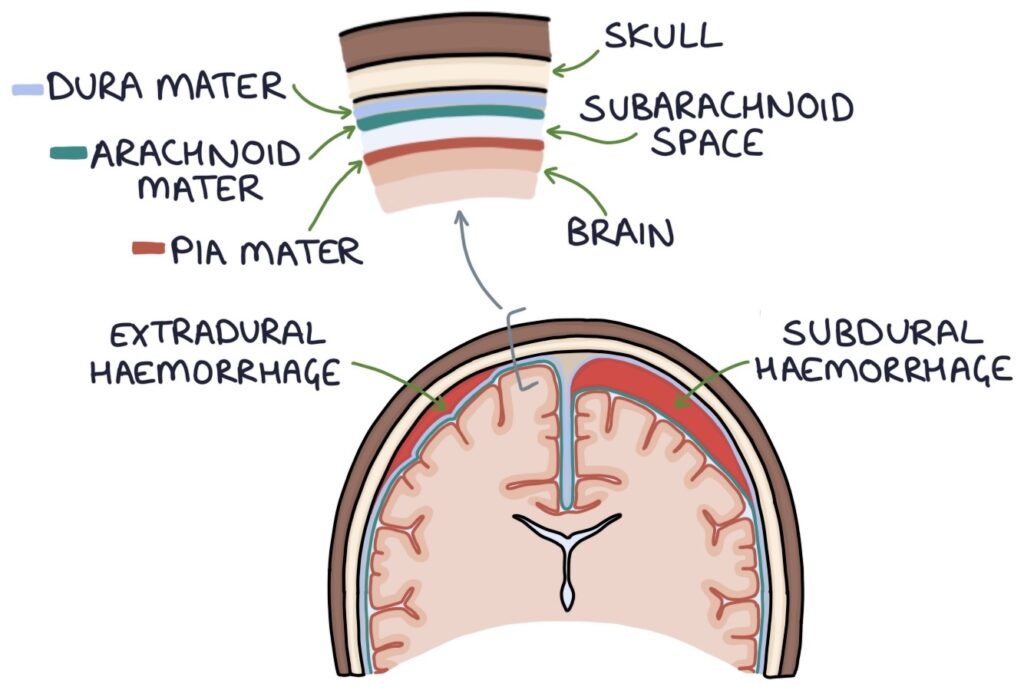
Subdural hemorrhage (SDH) occurs when bleeding develops in the subdural space, which lies between the dura mater (the brain’s tough outer membrane) and the arachnoid mater (the delicate middle layer). This bleeding typically results from torn bridging veins that connect the brain surface to the dural sinuses.
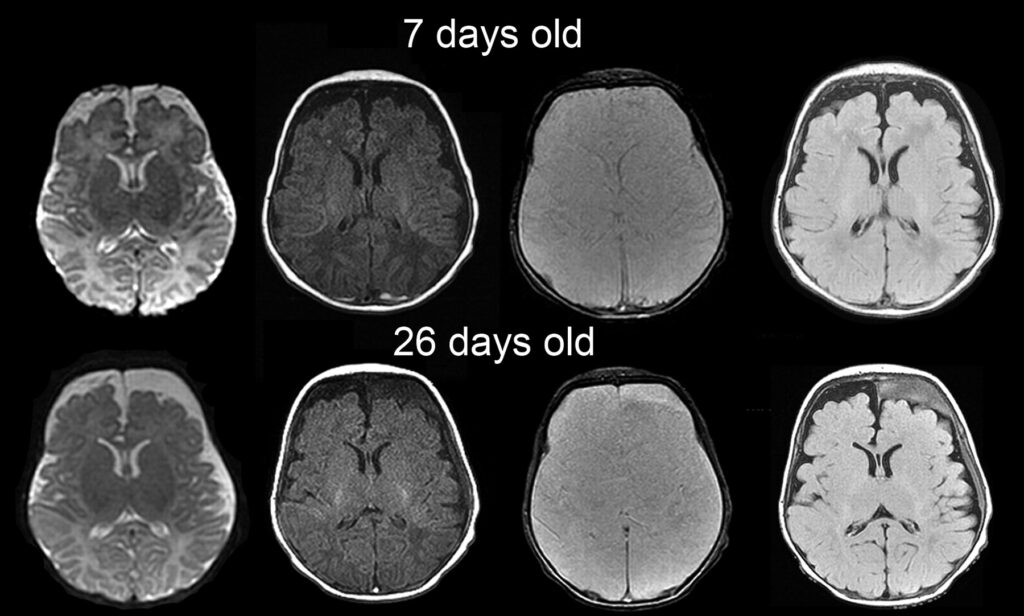
The condition manifests in three primary forms based on timing and presentation. Acute subdural hemorrhage develops within 72 hours of injury and appears hyperdense (bright) on CT scans. Subacute subdural hemorrhage occurs 3-21 days after trauma and shows isodense (similar to brain tissue) appearance on CT. Chronic subdural hemorrhage develops over weeks to months, appearing hypodense (dark) on imaging.
Understanding these distinctions is crucial because each type requires different management approaches and carries varying prognoses for patient recovery.
Anatomy and Pathophysiology: Subdural Hemorrhage
1. Formation and Development : Subdural Hemorrhage
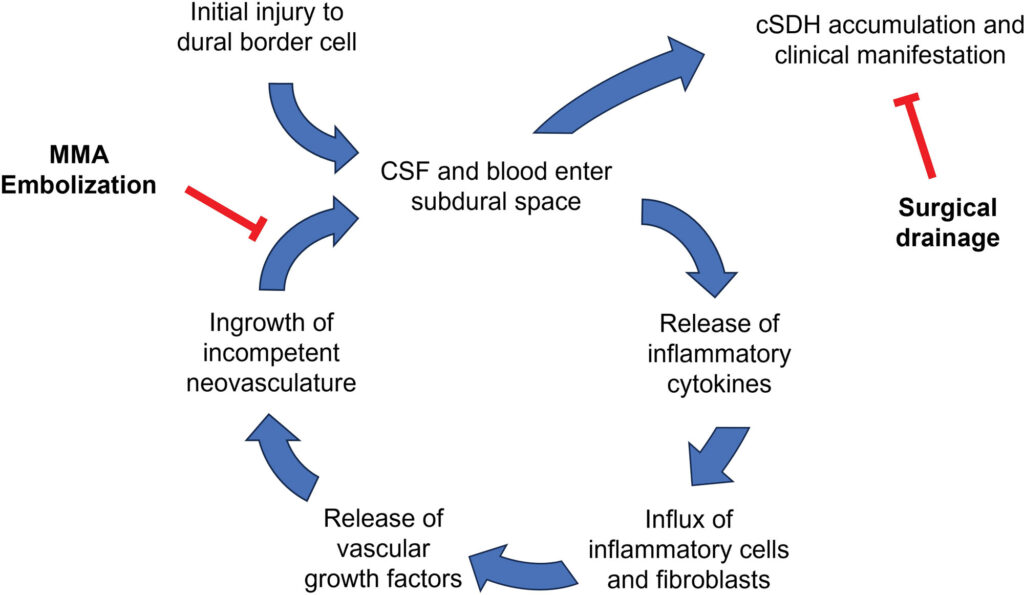
Subdural hemorrhage typically develops through two main mechanisms. Traumatic causes account for most cases, particularly following acceleration-deceleration injuries that stretch and tear bridging veins. These veins are vulnerable because they traverse from the brain surface through the subdural space to drain into venous sinuses.
Non-traumatic causes include coagulopathy, anticoagulant therapy, arteriovenous malformations, and spontaneous bleeding in elderly patients with brain atrophy. Brain shrinkage creates larger subdural spaces, making bridging veins more susceptible to rupture from minor trauma.
2. Location and Spread Patterns: Subdural Hemorrhage
Subdural blood typically accumulates over the cerebral convexity, following the brain’s surface contours. Unlike epidural hematomas, subdural hemorrhages cross suture lines and can extend over large brain areas. The bleeding often appears crescent-shaped on CT imaging, conforming to the brain’s surface rather than forming a lens-shaped mass.
The location affects clinical presentation significantly. Frontal subdural hemorrhages may cause personality changes and executive dysfunction, while parietal involvement can lead to sensory deficits and spatial neglect.
CT Imaging of Subdural Hemorrhage
1. Acute Phase Characteristics
CT subdural hemorrhage imaging shows distinct patterns that help determine timing and severity. Acute subdural hemorrhages appear hyperdense (brighter than brain tissue) on non-contrast CT scans due to fresh blood’s high protein content. The classic crescent or banana-shaped appearance distinguishes it from epidural hematomas, which typically show a biconvex or lens-shaped configuration.
Subdural hemorrhage CT images reveal several key features. First, the hemorrhage crosses suture lines, unlike epidural bleeding that stops at sutures. Second, mass effect may be present, causing midline shift, ventricular compression, or herniation patterns. Third, associated findings like cerebral edema, contusions, or skull fractures may be visible.
2. Subacute and Chronic Phases
Subacute subdural hemorrhages (3-21 days) become isodense to brain tissue, making detection challenging without contrast enhancement. Chronic subdural hemorrhages appear hypodense due to protein breakdown and CSF accumulation, often with septations or membranes visible.
CT angiography may help identify active bleeding sources, while repeat imaging monitors progression and guides treatment decisions.
Epidural vs Subdural Hemorrhage
Understanding the difference between epidural and subdural hemorrhage is crucial for proper diagnosis and treatment. These conditions have distinct anatomical locations, causes, and imaging appearances that affect patient outcomes.
1. Location and Anatomy
Epidural vs subdural hemorrhage locations differ significantly. Epidural hemorrhages occur between the skull and dura mater, while subdural hemorrhages develop between the dura and arachnoid layers. This anatomical difference creates characteristic imaging patterns.
Epidural hemorrhages typically result from arterial bleeding, often involving the middle meningeal artery following temporal bone fractures. Subdural hemorrhages usually involve venous bleeding from torn bridging veins.
2. Clinical Presentation Differences
Epidural hemorrhages often present with the classic “lucid interval” where patients initially appear normal before rapid deterioration. Subdural hemorrhages may show more gradual onset, particularly in chronic cases where symptoms develop slowly over weeks or months.
The mass effect patterns also differ. Epidural hematomas create focal compression, while subdural hemorrhages distribute over larger brain areas, potentially causing more diffuse symptoms.
Subarachnoid Hemorrhage vs Subdural Hematoma
The distinction between subarachnoid hemorrhage vs SDH involves different anatomical spaces and bleeding patterns. Subdural vs subarachnoid hemorrhage comparison reveals important diagnostic differences.
1. Anatomical Differences: Subdural Hemorrhage
Subarachnoid hemorrhage occurs in the space between the arachnoid and pia mater, where cerebrospinal fluid normally circulates. Subdural hematomas develop above this space, between the dura and arachnoid layers.
Subarachnoid bleeding often results from aneurysm rupture or arteriovenous malformation bleeding, while subdural hematomas typically follow trauma or occur spontaneously in elderly patients.
2. Imaging Characteristics: Subdural Hemorrhage
On CT imaging, subarachnoid hemorrhage appears as bright blood in the basal cisterns, , or ventricles. Subdural hematomas show the characteristic crescent shape over the brain surface. Blood distribution patterns help distinguish these conditions during emergency evaluation.
Clinical Significance and Management
Symptoms and Presentation
Subdural hemorrhage symptoms vary based on size, location, and acuity. Acute presentations include severe headache, altered consciousness, focal neurological deficits, and signs of increased intracranial pressure. Chronic subdural hemorrhages may cause subtle cognitive changes, gait disturbances, or gradual neurological decline.
Elderly patients are particularly susceptible to chronic subdural hemorrhages due to brain atrophy and increased fall risk. Anticoagulant therapy increases bleeding risk and complicates management decisions.
Treatment Approaches
Treatment depends on hemorrhage size, patient symptoms, and clinical condition. Small, asymptomatic subdural hemorrhages may be managed conservatively with serial imaging and neurological monitoring. Large or symptomatic collections require surgical evacuation through craniotomy or burr hole drainage.
Medical management includes reversing coagulopathy, controlling intracranial pressure, and preventing secondary complications like seizures or infections.
ICD-10 Coding for Subdural Hemorrhage
Proper documentation requires understanding SDH ICD 10 coding guidelines. The ICD 10 code for subdural hemorrhage varies based on timing, location, and underlying cause.
Primary Codes
The main hemorrhage subdural ICD-10 codes include:
- S06.5X – Traumatic subdural bleeding
- I62.0 – Nontraumatic subdural bleeding
- P10.0 – Subdural hemorrhage due to birth injury
Each code requires additional characters to specify laterality, encounter type, and associated complications.
Documentation Requirements
Accurate coding requires detailed documentation of:
- Traumatic versus nontraumatic etiology
- Acute, subacute, or chronic timing
- Associated consciousness level changes
- Surgical interventions performed
Proper coding ensures appropriate reimbursement and supports quality metrics for patient care outcomes.

Prevention and Risk Reduction
High-Risk Populations
Certain groups face increased subdural hemorrhage risk, including elderly patients, those on anticoagulation therapy, individuals with alcohol use disorders, and patients with bleeding disorders. These populations require careful monitoring and preventive strategies.
Fall prevention programs significantly reduce subdural hemorrhage risk in elderly populations. Safety measures include removing trip hazards, improving lighting, using assistive devices, and regular medication reviews.
Safety Measures
Helmet use during high-risk activities, vehicle safety practices, and workplace injury prevention reduce traumatic subdural hemorrhage incidence. Sports-related head injury protocols help identify at-risk athletes and prevent repeated trauma.
Medical management of anticoagulation therapy requires balancing bleeding risk with thromboembolism prevention, particularly in elderly patients with multiple risk factors.
Frequently Asked Questions
1. What is the difference between acute and chronic subdural hemorrhage?
Acute subdural hemorrhage occurs within 72 hours and appears bright on CT scans, while chronic develops over weeks to months and appears dark on imaging.
2. How is subdural hemorrhage diagnosed?
CT scanning is the primary diagnostic tool, showing characteristic crescent-shaped bleeding patterns that cross suture lines, distinguishing it from epidural hemorrhages.
3. What causes SDH?
Most cases result from trauma causing bridging vein tears, but spontaneous bleeding can occur with anticoagulation, brain atrophy, or vascular abnormalities.
4. When does SDH require surgery?
Surgery is indicated for large hemorrhages causing mass effect, neurological deterioration, or symptoms like persistent headaches and confusion.
5. Can SDH be prevented?
Prevention focuses on fall prevention in elderly patients, helmet use during high-risk activities, and careful anticoagulation management.
6. What is the prognosis for subdural hemorrhage?
Prognosis depends on hemorrhage size, patient age, and timing of treatment. Early recognition and appropriate management improve outcomes significantly.
7. How long does recovery take after SDH?
Recovery varies from weeks to months depending on severity, age, and complications. Some patients may have permanent neurological deficits.
Key Takeaways for Medical Practice
SDH represents a critical neurological emergency requiring prompt recognition and management. Understanding the anatomical basis, imaging characteristics, and clinical presentations helps healthcare providers deliver optimal patient care. CT imaging remains the gold standard for diagnosis, while proper ICD-10 coding ensures accurate documentation.
The distinction between subdural, epidural, and subarachnoid hemorrhages guides treatment decisions and patient counseling. Early intervention, when indicated, significantly improves patient outcomes and reduces long-term complications.
For medical students and healthcare providers, mastering SDH recognition and management is essential for emergency medicine, neurology, and neurosurgery practice. Continued education and clinical experience enhance diagnostic accuracy and treatment effectiveness.