Introduction
Organophosphorus compound poisoning remains a major emergency worldwide. These pesticides and nerve agents block acetylcholinesterase, the enzyme that clears acetylcholine. Therefore, acetylcholine rises at synapses and causes a cholinergic crisis. You may see miosis, wheeze, drooling, vomiting, and confusion. In severe cases, breathing fails.
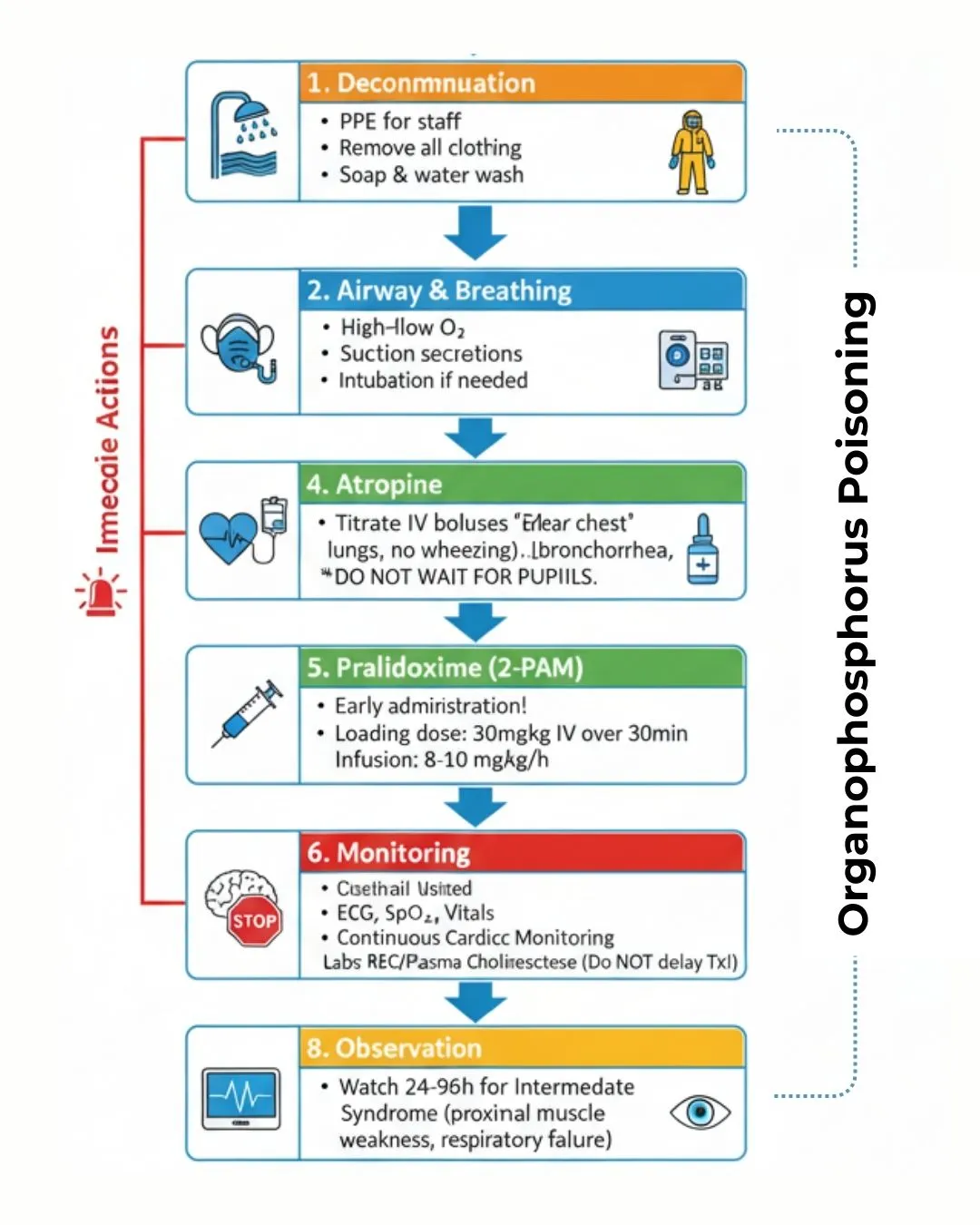
However, rapid steps save lives. First, decontaminate the patient and protect staff with PPE. Next, secure the airway and provide oxygen. Then, start atropine and titrate to clear the chest. After that, add pralidoxime (2-PAM) early to reactivate the enzyme. Finally, watch for the intermediate syndrome in the next 24–96 hours. For emergency basics on drugs and airway, review our airway and emergency drugs checklist.
In this guide, you will learn the mechanism, key signs, diagnosis, and a stepwise ED plan. You will also get dosing tables, exam-style notes, viva tips, and a simple diagram prompt.
What is organophosphorus compound poisoning?
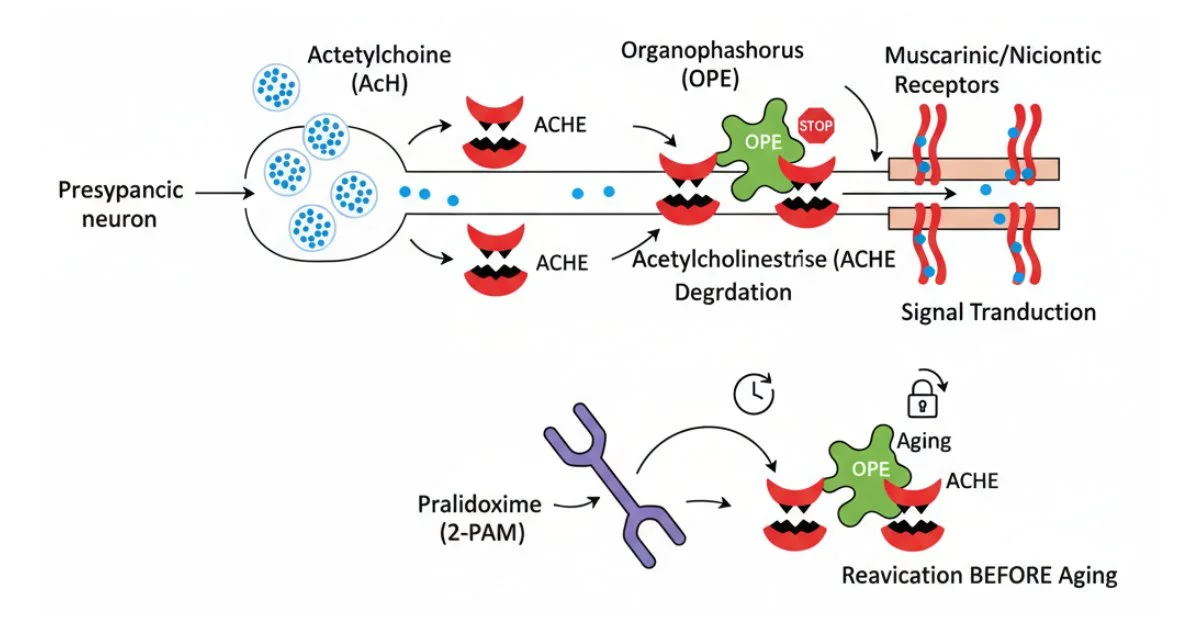
Organophosphorus compounds are common insecticides and warfare agents. They phosphorylate acetylcholinesterase (AChE) and stop it from working. As a result, acetylcholine builds up. Then, glands, smooth muscle, skeletal muscle, and the brain become over-stimulated.
The toxidrome spans muscarinic, nicotinic, and CNS features. Death usually occurs from airway obstruction and respiratory failure. Early recognition and protocol-driven care improve survival.
Takeaway: Think OP poisoning when there is pesticide exposure plus miosis, bronchorrhea, and wheeze. Treat first; confirm later. For a plain-language overview, see this peer-reviewed summary on OP poisoning
How OPs harm the body: AChE inhibition and “aging”
OPs bind to AChE at the active site. Initially, oximes like pralidoxime can remove the OP group. However, a chemical change called “aging” may occur. After aging, the bond becomes permanent. Therefore, oximes no longer work. Consequently, early oxime use matters.
Muscarinic, nicotinic, and CNS features
- Muscarinic (SLUDGE + BBB): salivation, lacrimation, urination, diarrhea, GI cramps, emesis; bronchorrhea, bronchospasm, bradycardia, miosis.
- Nicotinic: muscle fasciculations, weakness, tachycardia, and sometimes hypertension.
- CNS: agitation, seizures, coma, and central respiratory failure.
Clinical pearl: Respiratory failure from secretions and bronchospasm is the main killer. Therefore, atropinisation targets a dry chest and adequate ventilation.
First aid and ED management pathway
Scene and triage
- Ensure PPE for all responders. Equip all responders with PPE; for a quick refresher, see airway and emergency drugs.
- Move the patient to fresh air.
- Remove contaminated clothes and double-bag them.
- Wash hair and skin with soap and water. Avoid mouth-to-mouth.
ED priorities
-
Airway and Breathing: Give oxygen and suction secretions. Consider early intubation if there is persistent hypoxia, severe bronchorrhea, or fatigue. For a rapid refresher on resuscitation steps, read airway and emergency drugs.
- Circulation: Establish IV access and give fluids as needed.
- Decontamination: Continue thorough washing. Prevent secondary contamination of staff and equipment.
- Monitoring: Record SpO₂, ECG, BP, and respiratory rate. Send cholinesterase levels if available, but do not delay treatment.
- Glucose check: Exclude hypoglycemia early.
Antidote for organophosphorus compound poisoning: atropine and pralidoxime
Atropine reverses muscarinic effects. It dries secretions and relieves bronchospasm and bradycardia. Pralidoxime (2-PAM) reactivates AChE before aging occurs. Diazepam treats agitation and seizures.
Also, remember that carbamates may look similar but age less; management remains similar, with careful oxime use per local protocols.
Keyword note: This section intentionally includes the phrase antidote for organophosphorus compound poisoning to match search intent.
Doses, end-points, and controversies
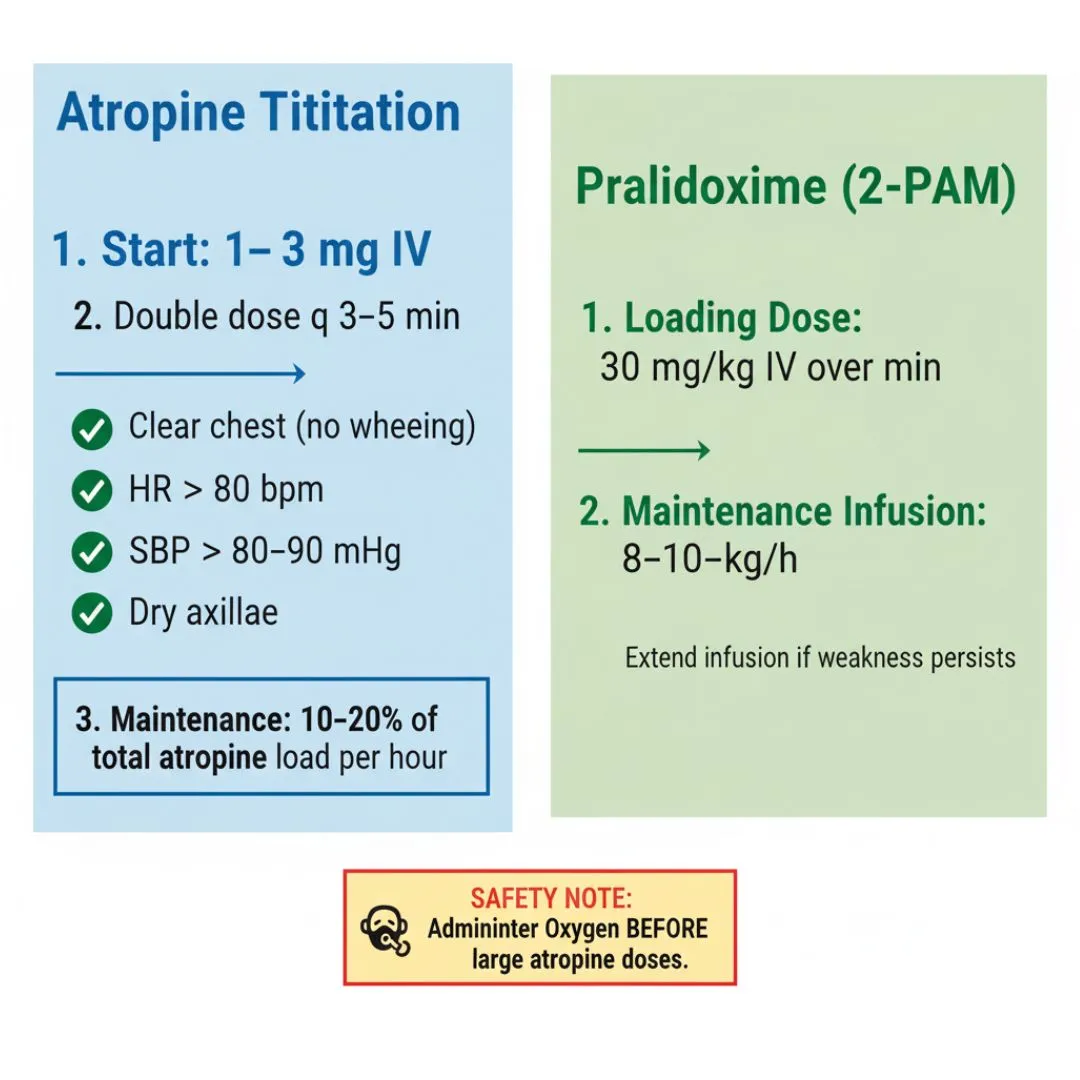
Table 1. Atropine titration (adult example)
| Step | Dose | Repeat | End-point |
|---|---|---|---|
| Start | 1–3 mg IV | Every 3–5 min, double dose | Clear chest, HR >80, SBP >80–90, dry axillae |
| Maintenance | 10–20% of total loading dose per hour | Titrate hourly | Maintain end-points without wet lungs |
Practical notes
- Give oxygen before large atropine doses to reduce arrhythmias.
- End-points beat fixed doses. Trust the clinical chest.
- Children require weight-based dosing; use pediatric references.
Table 2. Pralidoxime (2-PAM) dosing (adult example)
| Regimen | Dose |
|---|---|
| Loading | 30 mg/kg IV (max 2 g) over 30 min |
| Infusion | 8–10 mg/kg/h for 12–24 h; extend if weakness persists |
Controversies in oxime use
- Evidence for oximes varies across compounds and severity.
- Benefits are more likely with early administration and non-aged enzyme.
- Local guidelines should guide dosing and duration.
Reminder keyword: We again include organophosphorus compounds poisoning here to meet coverage goals.
Clinical relevance and complications
Intermediate syndrome (IMS) appears 24–96 hours after exposure. Patients develop neck flexor weakness, proximal limb weakness, and respiratory muscle weakness. Therefore, monitor vital capacity and be ready to ventilate.
OP-induced delayed polyneuropathy may occur weeks later. It causes distal weakness and numbness. Consequently, follow-up and rehabilitation are important. Need neuro red flags at a glance? Check our subdural hemorrhage quick guide.
High-risk clues
- Severe initial cholinergic crisis.
- Delayed oxime therapy.
- Prolonged atropine infusion needs.
Prevention and care (practical tips)
- Read labels and follow instructions exactly. To build safe habits while reading reports, try Widal test interpretation.
- Wear gloves, mask, goggles, and long sleeves.
- Mix and store chemicals away from food and children.
- Wash hands, body, and clothes after use.
- Do not reuse chemical containers.
- Seek medical help immediately if symptoms start.
Public-facing note: These steps reduce exposure for farmers, families, and responders. For antidote specifics, review pralidoxime guidance from HHS CHEMM
Exam-style Q&A
High-yield notes
- Define aging clearly and state its impact on oxime success.
- List atropinisation end-points: dry chest, HR >80, adequate BP.
- Give one adult 2-PAM loading example.
- State the IMS window and key signs.
- Contrast carbamate vs OP aging.
- Name one PPE step during decontamination.
Conclusion
OP poisoning is urgent yet treatable. Therefore, recognise the toxidrome early and follow a clear pathway. Then, decontaminate, protect staff, and atropinise to a dry chest. After that, add pralidoxime early and keep watch for intermediate syndrome. Finally, revise the exam pattern below and practise the diagram.
If you found this helpful, explore our other quick guides and exam notes on Simply MBBS.
Exam Question–Answer (University Pattern)
Exam stem (verbatim):
“Describe organophosphorus compound poisoning under (a) definition & mechanism, (b) clinical features, (c) management including antidotes, (d) applied/clinical aspects.”
Suggested marks (10): (a) 2, (b) 3, (c) 4, (d) 1.
Model answer
(a) Definition & mechanism — 2 marks
- OPs inhibit AChE, causing acetylcholine excess.
- Aging locks OP-AChE; oximes fail after aging.
(b) Clinical features — 3 marks
- Muscarinic: miosis, bronchorrhea, bronchospasm, bradycardia, SLUDGE.
- Nicotinic: fasciculations, weakness, tachycardia or hypertension.
- CNS: agitation, seizures, coma, respiratory failure.
(c) Management including antidotes — 4 marks
- PPE, decontamination, oxygen, suction, early intubation if required.
- Atropine IV, rapidly titrate to dry chest and stable vitals.
- Pralidoxime (2-PAM) early; loading then infusion.
- Diazepam for seizures; ICU monitoring; watch for IMS.
(d) Applied/clinical aspects — 1 mark
- Indications: cholinergic toxidrome after OP exposure.
- Tests: cholinesterase levels; do not delay therapy.
- Complications: IMS, delayed neuropathy.
Answer:
(a) Definition & Mechanism — 2 marks
Definition: Organophosphorus (OP) compounds are organic derivatives of phosphorus-containing acids that include pesticides, insecticides, and chemical warfare nerve agents. Organophosphorus poisoning occurs when these compounds inhibit acetylcholinesterase (AChE), leading to accumulation of acetylcholine and subsequent cholinergic toxicity.
Mechanism: OP compounds bind irreversibly to acetylcholinesterase by phosphorylating the serine hydroxyl residue at the active site of the enzyme. This inhibition prevents the normal breakdown of acetylcholine into choline and acetic acid, resulting in excessive accumulation of acetylcholine in cholinergic synapses throughout the central nervous system, peripheral nervous system, and neuromuscular junctions.
The aging process is crucial – over time, the organophosphate-AChE complex undergoes dealkylation, making the bond irreversible. Once aging occurs, oximes like pralidoxime become ineffective in reactivating the enzyme. The rate of aging varies with different compounds but can be as rapid as 1.3 minutes for nerve agents like soman.
(b) Clinical Features — 3 marks
Muscarinic Effects: The most prominent features result from overstimulation of muscarinic receptors and are remembered by the mnemonic SLUDGE (Salivation, Lacrimation, Urination, Defecation, Gastrointestinal motility, Emesis). Additional muscarinic signs include miosis (constricted pupils), bronchorrhea, bronchospasm, bradycardia, hypotension, and increased secretions.
Nicotinic Effects: These manifest as muscle fasciculations, weakness, cramps, twitching, and paralysis. Nicotinic stimulation can also cause tachycardia and hypertension through effects on sympathetic ganglia and adrenal medulla. Respiratory muscle weakness contributes significantly to respiratory failure.
Central Nervous System Effects: CNS manifestations include agitation, confusion, seizures, coma, and respiratory depression. The neurological effects result from acetylcholine accumulation in central cholinergic synapses and can progress to status epilepticus and respiratory arrest.
Time-Based Classification: Symptoms are categorized as acute (within 24 hours), delayed (24 hours to 2 weeks including intermediate syndrome), and late (beyond 2 weeks including delayed polyneuropathy).
(c) Management Including Antidotes — 4 marks
Initial Management: Immediate decontamination with personal protective equipment (PPE) to prevent secondary exposure. Ensure airway patency, provide oxygen supplementation, and suction excessive secretions. Early intubation may be required due to bronchorrhea, bronchospasm, and respiratory muscle weakness.
Atropine Therapy: Atropine is the primary antidote, acting as a competitive muscarinic receptor antagonist. Initial dose is 2-5 mg IV for adults (0.05 mg/kg for children), doubled every 3-5 minutes until “atropinization” is achieved. Signs of adequate atropinization include dry skin and mucosa, reduced secretions, no bronchospasm, tachycardia, and mydriasis. Severe cases may require hundreds of milligrams over days to weeks.
Pralidoxime (2-PAM): This oxime reactivates phosphorylated AChE by binding to the organophosphate. Loading dose is 30 mg/kg for adults (20-50 mg/kg for children) over 30 minutes, followed by continuous infusion at 8 mg/kg/hour for adults (10-20 mg/kg/hour for children). Must be administered before aging occurs, ideally within 24-48 hours, though delayed administration may still be beneficial for lipophilic compounds.
Seizure Management: Diazepam or other benzodiazepines for seizure control. Continuous monitoring in ICU setting is essential, with particular attention to respiratory status and potential for intermediate syndrome.
(d) Applied/Clinical Aspects — 1 mark
Clinical Indications: Diagnosis is based on cholinergic toxidrome following known or suspected OP exposure. The combination of muscarinic, nicotinic, and CNS effects following exposure to pesticides or nerve agents strongly suggests OP poisoning.
Diagnostic Tests: Red blood cell acetylcholinesterase levels are more specific and better correlated with poisoning severity than plasma cholinesterase levels. Normal cholinesterase levels are typically >3.93 U/ml, with levels <2 U/ml indicating significant poisoning. However, treatment should never be delayed while awaiting laboratory confirmation.
Complications: Intermediate Syndrome (IMS) occurs in approximately 20% of cases, developing 24-96 hours after initial recovery, characterized by respiratory muscle paralysis, proximal muscle weakness, and cranial nerve palsies. Organophosphate-Induced Delayed Polyneuropathy (OPIDP) is a rare complication occurring 2-4 weeks post-exposure, presenting as distal sensorimotor axonal neuropathy with progressive weakness, particularly affecting distal muscles and causing foot drop
Viva quick hits (one-liners)
- Define aging and its timeline.
- Two atropinisation end-points.
- Why oxygen before high-dose atropine?
- Adult 2-PAM loading dose example.
- IMS time window and key signs.
- One difference between carbamate and OP.
- Main cause of death in OP poisoning.
- One essential PPE step.
Last-minute revision checklist
- Recognise miosis + wet lungs quickly.
- Decontaminate early and protect staff.
- Atropine to dry chest, not to a number.
- Start pralidoxime before aging.
- Control seizures with benzodiazepines.
- Watch for IMS in 24–96 hours.
- Educate on safe pesticide handling.