Imagine walking into the ER at 3 AM. A 68-year-old patient presents with confusion. Her serum sodium is 118 mEq/L. Your heart races. This is hyponatremia in clinical practice—not just a lab value. It’s a potentially life-threatening emergency. Every year, hyponatremia affects up to 30% of hospitalized patients. This makes it the most common electrolyte disorder. Yet management errors remain frequent. These errors lead to complications ranging from brain damage to death. This guide equips medical students, physicians, and informed patients with evidence-based strategies. You’ll learn to recognize, diagnose, and treat hyponatremia safely and effectively.
What is Hyponatremia?
Hyponatremia in clinical practice means serum sodium falls below 135 mEq/L. This represents an imbalance between total body water and sodium. According to Harrison’s Principles of Internal Medicine (21st Edition), it’s the most frequent electrolyte abnormality. The condition occurs when water intake exceeds the kidney’s excretion capacity. It can also happen when sodium losses exceed intake.
Severity Classification:
- Mild: 130-135 mEq/L
- Moderate: 125-129 mEq/L
- Severe: <125 mEq/L
Timing Classification:
- Acute: <48 hours duration
- Chronic: ≥48 hours duration
This timing critically influences treatment strategies. It helps prevent neurological complications.
Why Understanding Hyponatremia Matters
Understanding hyponatremia in clinical practice carries profound implications. Patient outcomes depend on proper management. Healthcare quality improves with better knowledge.
Key Reasons It Matters:
-
Falls and Fractures: Even mild chronic hyponatremia increases fall risk by 67% in elderly patients. This leads to hip fractures and increased hospital stays.
-
Increased Mortality: Studies from 2024 show alarming statistics. Hospitalized patients with sodium <135 mEq/L have 2.5 times higher mortality rates. This occurs independent of underlying diseases.
-
Brain Complications: The brain swells when sodium drops rapidly. This causes cerebral edema. Symptoms include headache, confusion, seizures, and coma. Correcting too fast causes osmotic demyelination syndrome (ODS). This results in permanent neurological disability.
-
Healthcare Costs: Each hyponatremia episode adds $1,500-$3,200 in hospital charges. Extended stays and complications drive these costs.
-
Exam Importance: Board examinations consistently test hyponatremia pathophysiology. Students must master diagnostic algorithms. Residents need to differentiate SIADH from other causes.
Hyponatremia Pathophysiology
Normal Sodium Regulation
Hyponatremia pathophysiology starts with understanding normal balance. Serum sodium reflects a specific ratio. This is total body sodium plus potassium divided by total body water.
The Edelman Equation:
Serum Na+ = (Total Body Na+ + Total Body K+) / Total Body Wate
Three Key Kidney Mechanisms:
- Glomerular Filtration: Kidneys filter 180 liters daily
- Tubular Reabsorption: Reabsorb 99% of filtered sodium
- ADH-Mediated Water Reabsorption: Occurs in collecting ducts
ADH (Antidiuretic Hormone) Role:
Arginine vasopressin (AVP) is commonly called ADH. It’s the primary regulator of water balance. When plasma osmolality rises above 285 mOsm/kg, osmoreceptors trigger AVP release. AVP binds V2 receptors on collecting duct cells. This inserts aquaporin-2 water channels. Water reabsorption increases. Urine concentration reaches up to 1200 mOsm/kg. When plasma osmolality falls, AVP secretion stops. This allows dilute urine excretion (50-100 mOsm/kg).
Mechanisms Leading to Low Sodium
Hyponatremia pathophysiology involves two fundamental mechanisms. These are defective free water excretion or excessive water intake.
Three Defective Water Excretion Pathways:
- Non-osmotic AVP Release: ADH releases despite low serum osmolality. This prevents urinary dilution. Seen in SIADH, pain, nausea, and stress.
- Reduced Distal Tubular Fluid Delivery: Impairs diluting segment function. Occurs with decreased effective arterial blood volume. Examples include heart failure, cirrhosis, and nephrotic syndrome.
- Medication Effects: Drugs directly impair renal water handling. Thiazide-induced hyponatremia is most common. Thiazides block the Na-Cl cotransporter in the distal tubule. This is the kidney’s primary diluting site. It prevents maximum urine dilution. Simultaneously causes sodium losses. Stimulates AVP release through volume depletion.
Thiazide Statistics:
- Severe hyponatremia occurs in 4-11% of treated patients
- Highest risk: elderly women with low body mass
- Timing: typically within first two weeks of therapy
Read More : Approach to Unconscious Patient: Causes, Diagnosis, and Emergency Management
Types of Hyponatremia
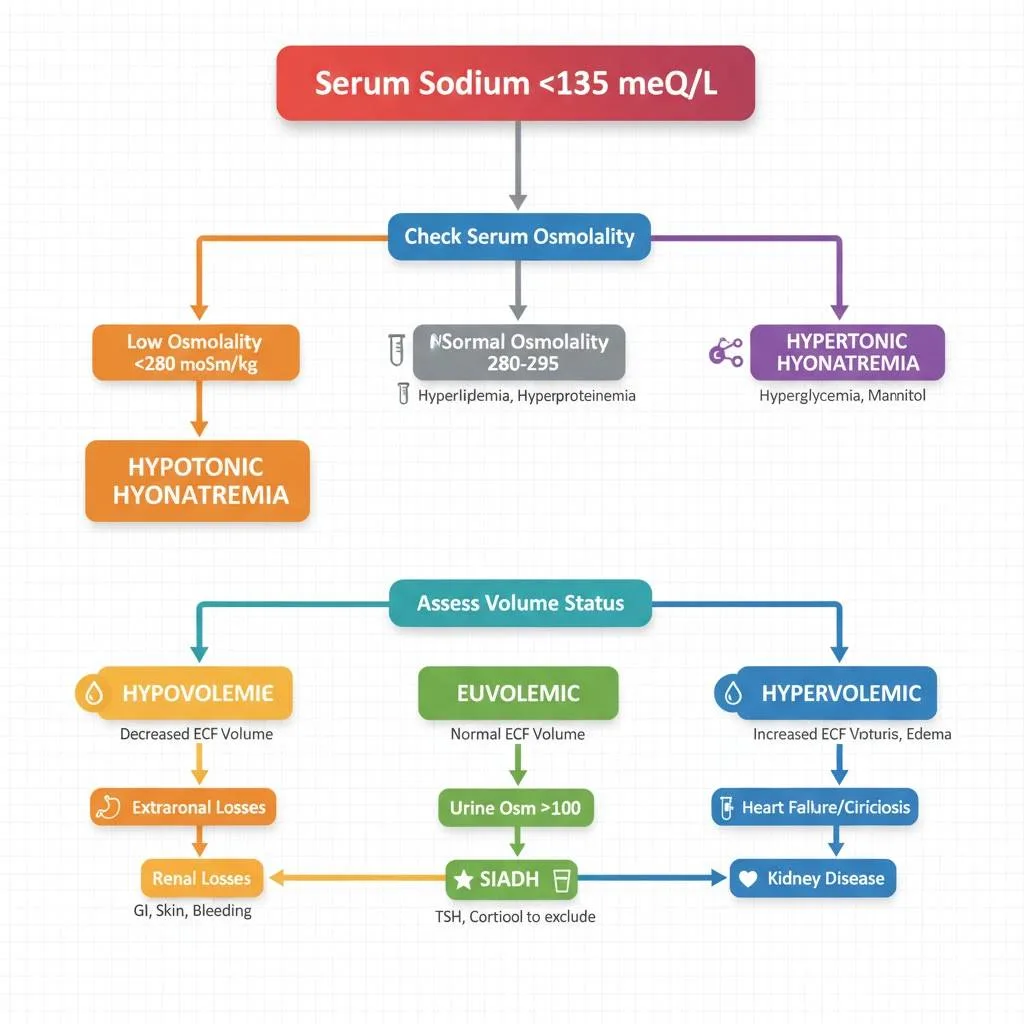
Types of hyponatremia are classified using a stepwise approach. This combines serum osmolality, volume status, and urine studies. Classification directly guides treatment decisions.
Hypovolemic Hyponatremia
Both total body sodium and water decrease. However, sodium losses exceed water losses.
Clinical Signs:
- Orthostatic hypotension
- Tachycardia
- Decreased skin turgor
- Dry mucous membranes
- Elevated BUN:creatinine ratio (>20:1)
Laboratory Findings:
- Serum osmolality <280 mOsm/kg
- Urine osmolality >100 mOsm/kg
- Urine sodium differentiates causes
Urine Sodium Interpretation:
High Urine Sodium (>40 mEq/L) indicates renal losses:
- Diuretics (especially thiazide-induced hyponatremia)
- Salt-wasting nephropathy
- Cerebral salt wasting
- Adrenal insufficiency
Low Urine Sodium (<20 mEq/L) suggests extrarenal losses:
- Vomiting
- Diarrhea
- Third-spacing (burns, pancreatitis)
- Excessive sweating
Treatment: Isotonic saline restores volume. This suppresses ADH. Allows water excretion.
Euvolemic Hyponatremia
Normal or slightly increased total body water occurs. Total body sodium remains normal. Results in dilutional hyponatremia without edema.
Physical Examination:
- Normal vital signs
- Normal jugular venous pressure
- No edema present
Laboratory Testing:
- Low serum osmolality (<280 mOsm/kg)
- Elevated urine osmolality (>100 mOsm/kg)
- Urine sodium typically >40 mEq/L
SIADH (Syndrome of Inappropriate ADH):
This represents the most common cause. Accounts for approximately 40% of hospital cases.
SIADH Diagnostic Criteria:
- Hypotonic hyponatremia (serum osmolality <280 mOsm/kg)
- Urine osmolality >100 mOsm/kg despite hypotonicity
- Urine sodium >40 mEq/L on normal salt intake
- Clinical euvolemia
- Normal thyroid, adrenal, and renal function
Common SIADH Causes:
- Small cell lung cancer
- CNS disorders (meningitis, stroke, trauma)
- Pulmonary disease (pneumonia, tuberculosis)
- Medications (SSRIs, carbamazepine, cyclophosphamide)
- Postoperative states
Other Euvolemic Causes:
- Primary polydipsia (urine osmolality <100 mOsm/kg)
- Hypothyroidism
- Adrenal insufficiency
Management: Fluid restriction <1 liter daily is first-line. Only 50% of SIADH patients respond adequately. Second-line therapies include oral urea, salt tablets, or vasopressin receptor antagonists.
Hypervolemic Hyponatremia
Increased total body sodium occurs. Total body water increases markedly. Manifests as edema despite low serum sodium.
Physical Findings:
- Peripheral edema
- Ascites
- Pulmonary crackles
- Elevated jugular venous pressure
- Hepatomegaly or cardiac enlargement
Common Causes:
- Heart Failure: Decreased cardiac output reduces effective arterial blood volume. Triggers ADH release. Urine sodium typically <20 mEq/L.
- Cirrhosis with Ascites: Splanchnic vasodilation reduces effective arterial volume. Stimulates ADH. Urine sodium usually <20 mEq/L.
- Nephrotic Syndrome: Hypoalbuminemia reduces plasma oncotic pressure. Reduces effective arterial volume. Urine sodium may exceed 20 mEq/L.
- Chronic Kidney Disease: GFR <30 mL/min impairs sodium and water excretion. Urine sodium typically >40 mEq/L.
Management Approach:
- Loop diuretics
- Fluid restriction (1-1.5 liters daily)
- Treat underlying condition
- Consider vasopressin antagonists for persistent cases
Hyponatremia Workup
The hyponatremia workup follows a systematic algorithm. This enables rapid cause identification. Prevents therapeutic errors.
Step 1: Initial Laboratory Assessment
Confirm True Hypotonic Hyponatremia:
- Order serum osmolality simultaneously with serum sodium
- Normal range: 285-295 mOsm/kg
Three Types Based on Osmolality:
Type 1 – Pseudohyponatremia:
- Normal osmolality (280-295 mOsm/kg) despite low sodium
- Caused by severe hyperlipidemia or hyperproteinemia
- Rare with modern analyzers
2 – Hypertonic Hyponatremia:
- Elevated osmolality (>295 mOsm/kg)
- Osmotically active substances draw water from cells
- Common causes: hyperglycemia, mannitol, radiocontrast
3 – True Hypotonic Hyponatremia:
- Low serum osmolality (<280 mOsm/kg)
- Requires further classification
Additional Initial Tests:
- Basic metabolic panel (BUN, creatinine, glucose, potassium)
- BUN:creatinine ratio >20:1 suggests hypovolemia
- BUN:creatinine ratio <10:1 suggests SIADH
- Serum uric acid (<4 mg/dL supports SIADH)
Step 2: Assess Volume Status
Clinical Assessment Methods:
- Orthostatic vital signs
- Skin turgor
- Mucous membrane moisture
- Jugular venous pressure
- Lung auscultation
- Edema presence
Combining multiple findings improves accuracy.
Step 3: Measure Urine Osmolality
Urine Osmolality <100 mOsm/kg:
- Indicates appropriately dilute urine
- Appropriate ADH suppression
- Suggests primary polydipsia or beer potomania
- Typically corrects spontaneously with solute intake
>100 mOsm/kg:
- Indicates inappropriate urinary concentration
- Demonstrates non-osmotic ADH release
- Or reduced distal delivery preventing dilution
- Occurs in most hyponatremia in clinical practice cases
- Requires volume status classification
Urine to Plasma Osmolality Ratio:
- Ratio >2 suggests SIADH
- Ratio <1 may indicate heart failure or cirrhosis
Step 4: Interpret Urine Sodium
In Hypovolemic Hyponatremia:
Urine Sodium >40 mEq/L indicates renal sodium wasting:
- Diuretics (especially thiazides)
- Mineralocorticoid deficiency
- Salt-wasting nephropathy
- Cerebral salt wasting
Urine Sodium <20 mEq/L suggests extrarenal losses:
- GI losses (vomiting, diarrhea)
- Skin losses (excessive sweating)
- Third-spacing
- Kidneys appropriately retain sodium
In Euvolemic Hyponatremia:
Urine Sodium >40 mEq/L supports SIADH diagnosis. Initial volume expansion triggers natriuresis. Fractional excretion of uric acid >12% provides support. Serum uric acid <4 mg/dL is typical.
Must Exclude:
- Hypothyroidism (check TSH)
- Adrenal insufficiency (morning cortisol, ACTH test)
In Hypervolemic Hyponatremia:
Urine Sodium <20 mEq/L indicates:
- Heart failure
- Cirrhosis
- Nephrotic syndrome
- Kidneys avidly retain sodium despite excess
Urine Sodium >40 mEq/L suggests:
- Advanced chronic kidney disease
- Active diuretic therapy
SIADH: Most Common Euvolemic Cause
SIADH (syndrome of inappropriate ADH) affects 30-40% of patients with low sodium. Understanding this condition is essential.
SIADH Pathophysiology
Non-osmotic AVP release occurs despite low plasma osmolality. Volume remains normal or expanded.
Mechanism:
- Excessive AVP binds V2 receptors in collecting ducts
- Promotes aquaporin-2 insertion
- Increases water reabsorption
- Produces concentrated urine despite plasma hypotonicity
- Retained water expands extracellular volume
- Suppresses renin-angiotensin-aldosterone
- Triggers atrial natriuretic peptide release
- Causes natriuresis until steady-state achieved
- Total body water increases by 4-7 liters
- Patients appear clinically euvolemic
Four SIADH Pathophysiological Patterns
Research from 2025 identified distinct patterns:
Type A (40-50% of cases):
- Persistently elevated AVP
- Regardless of osmolality
- Occurs with malignancies and pulmonary diseases
B (30-35% of cases):
- “Reset osmostat” pattern
- AVP suppression at lower osmotic thresholds
- Maintains stable mild hyponatremia (125-132 mEq/L)
C:
-
Abnormal AVP regulation only at low osmolalities
D:
- AVP-independent mechanisms
- V2 receptor mutations
- Ectopic antidiuretic substances
E (recently described):
- Linear copeptin decrease with rising osmolality
- May represent acute Type A resolution
Common SIADH Causes
Malignancies:
- Small cell lung cancer
- Head and neck cancers
- Lymphoma
Pulmonary Diseases:
- Pneumonia
- Tuberculosis
- Acute respiratory failure
CNS Disorders:
- Meningitis
- Encephalitis
- Stroke
- Hemorrhage
- Trauma
Medications:
- SSRIs (selective serotonin reuptake inhibitors)
- Carbamazepine
- Cyclophosphamide
- Vincristine
- NSAIDs
- Ecstasy
Other:
- Postoperative states
- HIV-related infections
- Age-related ADH dysregulation
SIADH Diagnosis
Required Criteria:
- Serum osmolality <280 mOsm/kg
- Serum sodium <135 mEq/L
- Urine osmolality >100 mOsm/kg (typically >300)
- Urine sodium >40 mEq/L
- Clinical euvolemia
- Normal thyroid function
- Normal adrenal function
- Normal cardiac function
- Normal hepatic function
- Normal renal function
Supportive Findings:
- Hypouricemia (<4 mg/dL)
- Low BUN (<10 mg/dL)
- Fractional excretion of uric acid >12%
Must Exclude:
- Hypothyroidism (check TSH)
- Adrenal insufficiency (morning cortisol >18 μg/dL)
Read More : Heart Failure: Classification, Diagnosis & Notes
Thiazide-Induced Hyponatremia
Thiazide-induced hyponatremia is one of the most common iatrogenic disorders. It accounts for 20-30% of severe hospital-acquired hyponatremia.
Why Thiazides Cause Hyponatremia
Thiazide diuretics are first-line antihypertensives. However, they cause hyponatremia through multiple mechanisms.
Three Main Mechanisms:
- Block Diluting Segment: Thiazides block the Na-Cl cotransporter (NCC). This occurs in the distal convoluted tubule. This is the nephron’s primary urinary diluting segment. Blockade prevents sodium reabsorption without water. Impairs maximum urinary dilution. Raises minimum urine osmolality from 50 to 150-250 mOsm/kg.
- Stimulate ADH Release: Thiazide-induced sodium losses cause volume contraction. This stimulates non-osmotic ADH release. Promotes water retention despite hypotonicity.
- Increase Collecting Duct Permeability: Studies show thiazides may increase water permeability. This occurs through aquaporin-2 upregulation. Further impairs water excretion.
Why Not Loop Diuretics?
Loop diuretics rarely cause severe hyponatremia. They block the thick ascending limb. This is the concentrating segment, not the diluting segment. Loop diuretics impair urinary concentration. They promote free water excretion. This protects against hyponatremia development.
Risk Factors
Thiazide-induced hyponatremia occurs in 4-11% of treated patients. Certain populations show significantly higher risk.
High-Risk Groups:
- Elderly age (>70 years)
- Female sex (2-3 times higher incidence)
- Low body weight or BMI <23 kg/m²
- Concurrent medications (SSRIs, NSAIDs, opioids)
- Low dietary solute intake
Timing:
- 50-90% of cases occur within two weeks of starting therapy
- Can develop anytime when additional risk factors emerge
Clinical Presentation
Range of Symptoms:
Mild Cases (130-135 mEq/L):
- Asymptomatic
- Discovered on routine labs
Severe Cases (<125 mEq/L):
- Confusion
- Weakness
- Nausea
- Seizures
- Coma
Important Note: Sodium can fall precipitously within hours to days. Susceptible individuals develop acute symptomatic hyponatremia. This requires emergency treatment.
Laboratory Findings
Typically mimics SIADH:
- Low serum osmolality
- Urine osmolality >100 mOsm/kg (often >300)
- Urine sodium >40 mEq/L
- Low-normal BUN and creatinine
- Hypouricemia
Volume Status Differentiation:
Frank Hypovolemia:
- Orthostatic hypotension present
- Elevated BUN:creatinine ratio
- Responds to isotonic saline
Apparent Euvolemia:
- Resembles SIADH
- Retained water masks volume depletion
- May not respond to isotonic saline
- Risk of overcorrection with saline
Management Strategy
Treatment depends on severity and symptoms.
Acute Symptomatic Cases:
- Stop thiazide immediately
- Administer 3% hypertonic saline: 100-150 mL boluses
- Target: 4-6 mEq/L sodium increase to resolve symptoms
- Monitor: Sodium every 2-4 hours
- Maintain correction rate: ≤10-12 mEq/L in 24 hours
- High-risk patients: ≤8 mEq/L in 24 hours
Asymptomatic or Mild Cases:
- Stop thiazide
- Restrict fluids to <1 L daily
- Encourage normal salt diet
- Replete potassium aggressively
- Monitor sodium closely
Prevention Strategies:
- Identify high-risk patients before starting therapy
- Use lowest effective doses (12.5-25 mg vs 50 mg)
- Check sodium within 1-2 days in elderly women
- Check sodium in small individuals early
- Educate patients about avoiding excessive water
Safe Alternative:
Loop diuretics represent safer alternatives. They rarely cause severe hyponatremia. Consider switching in patients who develop thiazide-induced hyponatremia.
Hyponatremia Treatment Guidelines
Hyponatremia treatment guidelines have evolved significantly. 2024-2025 updates emphasize individualized correction rates. Safety protocols prevent osmotic demyelination syndrome.
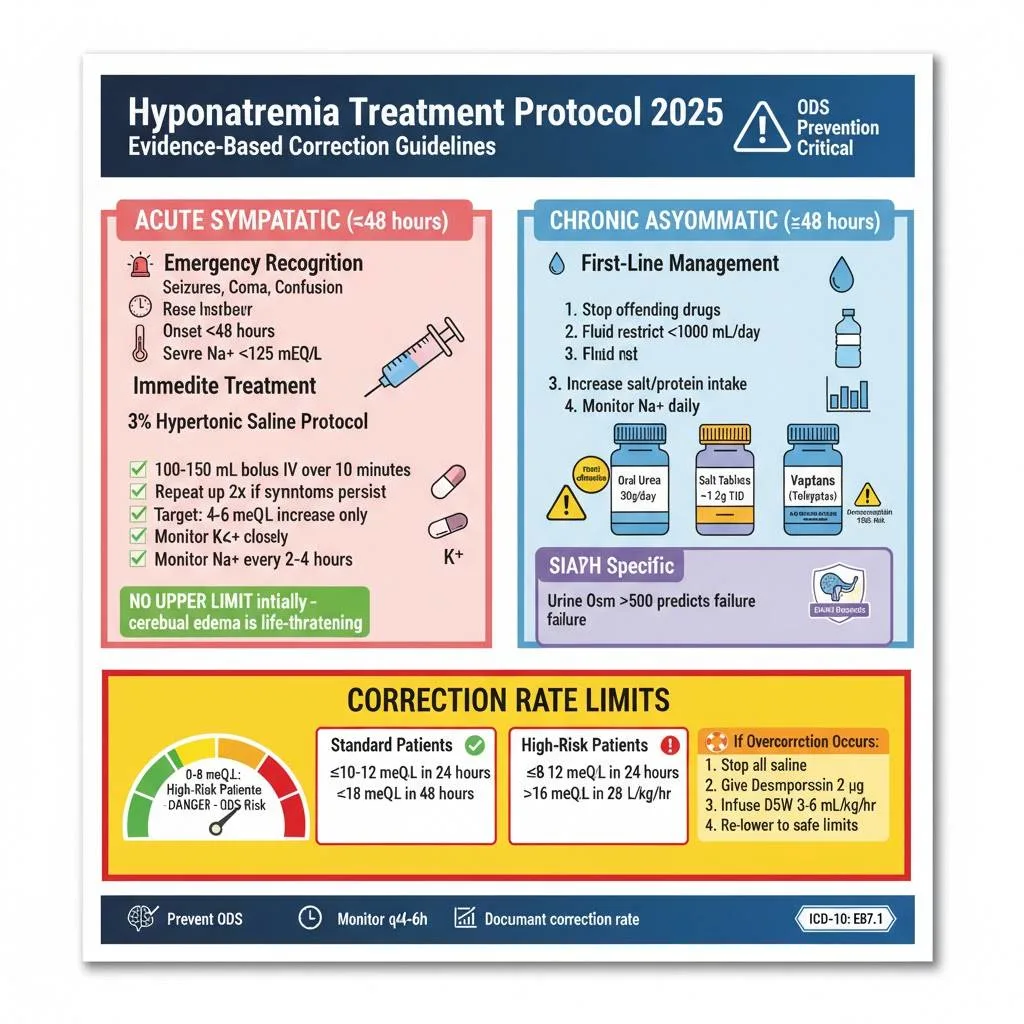
Acute Symptomatic Management
Acute symptomatic hyponatremia is a neurological emergency. Requires immediate intervention.
Why It’s Dangerous:
When sodium drops rapidly (<48 hours), neurons cannot adapt. They can’t extrude organic osmolytes adequately. Results in cerebral edema.
Symptoms of Cerebral Edema:
- Headache
- Nausea and vomiting
- Confusion
- Lethargy
- Seizures
- Respiratory distress
- Coma
Young women show particular vulnerability. Possibly due to hormonal influences.
First-Line Treatment:
Hypertonic Saline for Hyponatremia (3% solution = 513 mEq/L sodium)
2024 Recommended Protocol:
- Give 100-150 mL boluses IV
- Infuse over 10-15 minutes
- Repeat up to two additional times if severe symptoms persist
- Each 100 mL bolus raises sodium approximately 1-2 mEq/L (70 kg patient)
- Target 4-6 mEq/L increase to reverse cerebral edema
- Monitor sodium every 2-4 hours
Alternative Protocol:
- Continuous 3% saline infusion at 15-30 mL/hour
- Recent studies favor bolus administration
- Achieves faster symptom resolution
- Lower overcorrection rates (41% vs 57%)
Body Weight-Adjusted Dosing:
For smaller individuals (particularly Asian populations):
- Consider 1-2 mL/kg boluses
- Prevents excessive correction
Adrogue-Madias Formula:
Estimates sodium change from infusions:
Δ Serum Na+ = (Infusate Na+ – Serum Na+) / (Total Body Water + 1)
Where:
- TBW = 0.6 × body weight (men)
- TBW = 0.5 × body weight (women)
Note: Formula underestimates response during aquaresis.
Additional Measures:
Add Furosemide 20-40 mg IV:
- Enhances free water excretion
- Prevents volume overload
- Especially important in elderly patients
- Critical in heart failure patients
Monitor Potassium Closely:
- Hypokalemia accelerates sodium correction
- Edelman equation includes potassium in numerator
When to Stop:
Once symptoms resolve, stop hypertonic saline. Reassess patient status. Continued aggressive correction increases ODS risk.
Important Exception:
Acute symptomatic cases merit no upper correction rate limit initially. Mortality from untreated cerebral edema exceeds ODS risk. However, prudent monitoring remains essential.
Chronic Asymptomatic Management
Chronic hyponatremia (≥48 hours) allows cerebral adaptation. Neurons extrude organic osmolytes. These include glutamate, taurine, and myo-inositol. Reduces brain edema despite persistent hypotonicity.
Danger of Rapid Correction:
Osmotic demyelination syndrome (ODS) can occur. Neurons cannot regenerate osmolytes quickly enough. Causes white matter injury.
ODS Affects:
- Pons
- Basal ganglia
- Cerebellum
ODS Symptoms (appear 2-6 days post-correction):
- Dysarthria
- Dysphagia
- Quadriparesis
- Behavioral changes
- Locked-in syndrome
- Often permanent damage
First-Line Conservative Measures:
-
Address Underlying Causes:
-
Stop offending medications
-
Treat hypothyroidism
-
Treat adrenal insufficiency
-
Manage heart failure or cirrhosis
-
-
Implement Fluid Restriction:
-
<1000 mL/day
-
Or 500 mL below 24-hour urine output
-
-
Increase Dietary Intake:
-
Increase sodium intake
-
Increase protein intake
-
Solute loading promotes osmotic diuresis
-
-
Encourage Normal Activity
Predictors of Fluid Restriction Failure:
Fluid restriction corrects only 40-50% of SIADH cases.
Failure Indicators:
-
Urine osmolality >500 mOsm/kg
-
Urine (Na+ + K+) exceeds serum sodium
-
24-hour urine volume <1500 mL
-
<2 mEq/L sodium rise after 24-48 hours
These patients require second-line therapies.
Second-Line Therapies:
1. Oral Urea (15-60 g/day):
- Start with 30 g/day in divided doses
- Highly effective second-line treatment
- Induces osmotic diuresis
- Free water excretion exceeds 500 mL per 15 g urea
- Compare to just 42 mL per 1 gram salt tablet
- 64% achieve sodium ≥130 mEq/L within 72 hours
Limitations:
- Bitter taste limits acceptability
- Dissolve in sweet beverages or juice
- Can cause overcorrection
- Highest risk in elderly with baseline sodium <120 mEq/L
- Unavailable as FDA-approved medication in US
- Available in Europe
2. Salt Tablets (1-2 grams TID):
- Combined with fluid restriction
- Increase solute intake
- Promotes free water excretion
- Less effective than urea
3. Loop Diuretics (Furosemide 20-40 mg daily):
- Plus salt replacement
- EFFUSE-FLUID trial showed no significant advantage
- Increased hypokalemia trends
- Increased AKI trends
Hypertonic Saline Protocol for Chronic Cases
Beyond emergency management, hypertonic saline for hyponatremia helps chronic symptomatic cases. Use when conservative measures fail.
Calculate Sodium Deficit:
Na+ deficit = 0.6 × body weight × (target Na+ – current Na+)
Note: Provides rough estimates only.
2024 Sterns Protocol:
- Administer 3% saline continuous infusion
- Calculate rates achieving target correction rate
- Give simultaneous desmopressin (2 μg IV/SC every 6-8 hours)
- Check sodium every 4-6 hours initially
- Then every 6-8 hours once stable
Why Desmopressin?
Renders patients antidiuretic. Prevents unpredictable secondary aquaresis. Aquaresis commonly causes overcorrection. Occurs when ADH suddenly suppresses. Happens after reaching sodium thresholds. Or when underlying causes resolve.
Titration Strategy:
Titrate saline rate targeting safe correction limits. Desmopressin prevents aquaresis. Stop both once target reached.
Alternative Approach:
- Infuse 3% saline until reaching daily limits
- Switch to D5W (5% dextrose in water)
- Rate matches ongoing urine output
- Prevents further rises
If Aquaresis Develops:
Signs:
- Urine output suddenly >100 mL/hour
- Falling urine osmolality (<200 mOsm/kg)
Action:
- Start desmopressin immediately
- Monitor closely
Weight-Adjusted Dosing:
3% saline at 1 mL/kg/hour provides safer alternative. Especially in small individuals. Compared to fixed-rate protocols.
Hyponatremia Correction Rate Safety
Safe hyponatremia correction rate limits prevent osmotic demyelination. Allow adequate treatment simultaneously.
Current 2024-2025 Guidelines:
Most Patients:
- <10-12 mEq/L in any 24-hour period
- <18 mEq/L in any 48-hour period
High-Risk Patients:
- <8 mEq/L in 24 hours
- <16 mEq/L in 48 hours
High-Risk Criteria:
- Serum sodium <120 mEq/L
- Chronic severe malnutrition
- Alcoholism
- Cirrhosis
- Hypokalemia
Exception:
Acute symptomatic hyponatremia with severe symptoms. These include seizures or coma. Requires no initial upper limit. Immediate mortality from cerebral edema exceeds ODS risk. Target 4-6 mEq/L to resolve symptoms. Then stop aggressive treatment.
Recent Study Findings:
Large retrospective studies found overcorrection (>8 mEq/L in 24 hours). Occurred in 18-41% of severe cases. However, ODS developed in only 0.05-0.5%. Suggests current limits may be overly conservative. However, existing guidelines remain standard of care. Important for medicolegal and patient safety purposes.
If Overcorrection Occurs:
Implement rescue therapy immediately. Reduces ODS risk.
Rescue Therapy Steps:
- Stop all sodium-containing fluids
- Stop hypertonic saline
- Administer desmopressin (2 μg IV/SC every 6-8 hours)
- Infuse D5W at 3-6 mL/kg/hour for 2-4 hours
- Continue until sodium falls back to correction limit
- Re-check and adjust
Target:
Re-lower sodium to appropriate 24-hour limit:
- 10-12 mEq/L rise from initial value (most patients)
- 8 mEq/L in high-risk patients
2024 Consensus:
Rescue therapy recommended primarily for:
- Severe hyponatremia (≤125 mEq/L)
- Correcting >10 mEq/L in 24 hours
- Patients at high ODS risk
Vasopressin Receptor Antagonists
Vasopressin receptor antagonists (vaptans) like tolvaptan effectively raise sodium. Work in SIADH, heart failure, and cirrhosis.
Mechanism:
Selective V2 receptor blockade. Causes aquaresis (water excretion without sodium).
Dosing:
Tolvaptan 15 mg daily initially.
Significant Risks:
Overcorrection is common:
- 8 mEq/L rise in 24 hours occurs in 25-45%
- Higher risk with low baseline sodium
- Higher risk with malignancy
- Higher risk with low body weight
- Higher risk with concurrent other treatments
Required Monitoring:
- Hospitalization mandatory when initiating
- Intensive monitoring required
- Sodium every 6-12 hours initially
- Allow free water access
- Provide IV D5W if needed for re-lowering
Current Status:
- FDA approved
- Expensive ($300-500/day)
- Reserved for refractory cases
- Used after conservative measures fail
- No mortality benefit data available
Hyponatremia ICD-10 Coding
Accurate hyponatremia ICD-10 coding ensures appropriate reimbursement. Facilitates quality metrics tracking. Supports epidemiological research.
Primary Code
ICD-10 code for hyponatremia: E87.1
Full description: E87.1: Hypo-osmolality and hyponatremia
Includes disorders of plasma sodium balance. Results in low serum sodium <135 mEq/L.
Additional Specificity
ICD-10 hyponatremia coding requires additional specificity when possible.
Examples:
Thiazide-Induced:
- E87.1 (primary)
- Plus T50.2X5 (Adverse effect of diuretics)
SIADH:
- E87.1 (primary)
- Plus E22.2 (SIADH)
Newborns:
- P74.22 (Neonatal hyponatremia)
- Not E87.1
Related Codes
Underlying Conditions:
- E86.0 (Dehydration) – hypovolemic cases
- I50.9 (Heart failure) – hypervolemic cases
- K70.11 (Alcoholic hepatitis with ascites) – cirrhosis
- N04.9 (Nephrotic syndrome) – as appropriate
Complications:
- G93.6 (Cerebral edema) – acute symptomatic
- G37.2 (Central pontine myelinolysis) – if ODS develops
Documentation Importance
Hyponatremia ICD-10 code E87.1 applies across all severities. ICD-10-CM lacks severity modifiers.
Clinical Documentation Should Specify:
- Severity (mild, moderate, severe)
- Chronicity (acute vs. chronic)
- Symptom status (asymptomatic vs. symptomatic)
- Causative factors
Document in narrative notes. Even when not separately coded.
Benefits of Proper Coding:
- Case-mix adjustment
- Hospital comparison metrics
- Reimbursement optimization
- Medical knowledge advancement
- Coded data analytics
Common Mistakes to Avoid
Medical errors in hyponatremia in clinical practice cause preventable harm. Recognizing pitfalls enables safer management.
7 Most Common Errors:
1. Correcting Too Rapidly
Most dangerous error. Causes irreversible osmotic demyelination syndrome.
Rules:
- Never exceed 10-12 mEq/L in 24 hours (most patients)
- Never exceed 8 mEq/L in 24 hours (high-risk patients)
- Exception: acute symptomatic emergencies
Prevention:
- Check sodium every 4-6 hours during active treatment
- Detect unexpected rises early
- Particularly important with isotonic saline in hypovolemic cases
- Secondary aquaresis causes rapid overcorrection
2. Using Normal Saline in SIADH
Worsens hyponatremia rather than correcting it.
Why It Fails:
When urine osmolality exceeds plasma osmolality, normal saline becomes hypotonic. Normal saline contains 154 mEq/L sodium. This is hypotonic relative to concentrated urine. Adds more free water than sodium. Lowers serum sodium further.
Correct Approach:
- Restrict fluids instead
- Or use hypertonic saline if correction needed
3. Failing to Stop Offending Medications
Allows continued hyponatremia. Other interventions become ineffective.
Action Required:
Systematically review all medications. Discontinue implicated drugs:
- Thiazides
- SSRIs
- Carbamazepine
- NSAIDs
- Other known causes
4. Ignoring Potassium
Leads to unexpected overcorrection.
Edelman Equation:
Includes both sodium and potassium in numerator. Potassium repletion in hypokalemic patients raises serum sodium simultaneously.
Action Required:
Account for potassium when calculating correction rates.
5. Missing Cortisol or Thyroid Deficiency
Allows dangerous conditions to persist untreated.
Action Required:
Always check in unexplained hyponatremia:
- TSH (thyroid function)
- Morning cortisol (adrenal function)
Hypothyroidism and adrenal insufficiency mimic SIADH. However, they require hormone replacement.
6. Inadequate Follow-Up
Discharging patients on fluid restriction without follow-up. Risks recurrent symptomatic episodes.
Action Required:
- Arrange outpatient sodium checks within one week
- Educate patients about symptoms requiring emergency evaluation
- Involve family members in monitoring
- Arrange home health services for high-risk patients
- Especially important for elderly patients
- Critical for those with multiple comorbidities
7. Starting Tolvaptan Without Monitoring
Allows unpredictable aquaresis. Commonly causes dangerous overcorrection.
Requirements:
Vaptans require:
- Inpatient initiation
- Sodium checks every 4-6 hours for 24-48 hours
- Close monitoring throughout
Outpatient vaptan use without proper monitoring has caused permanent neurological injury. Results from undetected overcorrection.
Best Practice:
Adhere to protocol-driven care. Utilize institutional hyponatremia order sets. Reduces error rates significantly.
Read More : Pneumonia: Clinical Approach, Diagnosis & Management
Frequently Asked Questions (FAQs) About Hyponatremia
Q : How fast should hyponatremia be corrected safely?
Safe hyponatremia correction rate limits are ≤10-12 mEq/L in 24 hours. Also ≤18 mEq/L in 48 hours for most patients. High-risk patients need slower correction. These include sodium <120, alcoholism, cirrhosis, or malnutrition. They should be corrected ≤8 mEq/L in 24 hours. This prevents osmotic demyelination syndrome.
Q : When should 3% hypertonic saline be used?
Hypertonic saline for hyponatremia treats acute symptomatic cases. Use for seizures, coma, or severe altered mental status. Give 100-150 mL boluses IV. Target 4-6 mEq/L sodium increase to resolve symptoms. Monitor sodium every 2-4 hours closely.
Q : What differentiates SIADH from cerebral salt wasting?
SIADH presents with euvolemia. Cerebral salt wasting shows hypovolemia with high urine sodium. Both occur with CNS pathology. Volume status assessment differentiates them. Response to fluid administration is key. Cerebral salt wasting improves with isotonic saline. SIADH worsens with normal saline.
Q : Can normal saline worsen hyponatremia?
Yes, in SIADH or other euvolemic causes. This happens when urine osmolality greatly exceeds plasma osmolality. Normal saline (154 mEq/L) becomes hypotonic. Relative to patient’s concentrated urine, it adds more free water than sodium. Paradoxically lowers serum sodium further.
Q : What causes thiazide-induced hyponatremia?
Thiazide-induced hyponatremia develops from blocking the distal tubule Na-Cl cotransporter. This is the diluting segment. Blockade impairs urinary dilution. Also causes sodium losses. Stimulates ADH release. Risk is highest in elderly women. Typically occurs within first two weeks of therapy.
Q : What labs differentiate hyponatremia types?
Key tests include serum osmolality (confirms hypotonic). Also urine osmolality (assesses ADH activity). Urine sodium (differentiates renal vs. extrarenal losses). Volume status (clinical assessment). BUN/creatinine ratio and serum uric acid. This hyponatremia workup algorithm identifies underlying cause.
Q : How is SIADH diagnosed?
SIADH diagnosis requires low serum osmolality (<280). Inappropriately concentrated urine (>100 mOsm/kg). Urine sodium >40 mEq/L. Clinical euvolemia. Must exclude hypothyroidism, adrenal insufficiency, and diuretics. Also exclude renal, cardiac, and hepatic disease. Hypouricemia (<4 mg/dL) supports diagnosis.
Exam Questions: University Pattern
Question 1: Short Essay (10 Marks)
Scenario:
A 72-year-old woman presents to ED with confusion. Serum sodium is 118 mEq/L. She started hydrochlorothiazide 25 mg daily two weeks ago. Blood pressure is 110/70 mmHg lying, 105/68 sitting. Heart rate 88 regular. No edema present. Labs show K+ 3.2 mEq/L, urine osmolality 420 mOsm/kg. Urine sodium 48 mEq/L.
Question: Outline your diagnostic approach and immediate management plan.
Model Answer (10 marks):
Diagnosis (3 marks):
This is thiazide-induced hyponatremia. Hydrochlorothiazide started 2 weeks prior (typical timing). Severe hyponatremia present (sodium <125 mEq/L). Symptomatic presentation with confusion. Volume status appears euvolemic to mildly hypovolemic. Minimal orthostatic changes noted. No edema present. Lab pattern mimics SIADH. Inappropriately concentrated urine (420 mOsm/kg). Elevated urine sodium (48 mEq/L). Hypokalemia (3.2 mEq/L) common with thiazides. Contributes to hyponatremia severity.
Immediate Management (5 marks):
Stop hydrochlorothiazide immediately (1 mark)
Check additional labs: Serum osmolality, BUN, creatinine, glucose, uric acid. Also TSH and cortisol levels (1 mark)
Hypertonic saline 3%: Give 100 mL IV bolus over 10 minutes. May repeat once if confusion persists. Target 4-6 mEq/L sodium increase initially (2 marks)
Potassium repletion: Aggressive KCl replacement to goal K+ >4.0 mEq/L. Potassium correction contributes to sodium rise per Edelman equation (1 mark)
Monitor sodium every 2-4 hours: Ensure correction rate ≤8-10 mEq/L in 24 hours. Prevents osmotic demyelination. High-risk patient due to elderly age, severe hyponatremia, hypokalemia (1 mark)
Supportive care: Fluid restriction once acute symptoms resolve. Normal salt diet. Monitor neurological status. Seizure precautions as needed.
Further Steps (2 marks):
Once stable, transition to loop diuretic (furosemide). If diuretic still needed, loop diuretics rarely cause severe hyponatremia. Outpatient follow-up with sodium check within 3-5 days. Patient education on avoiding excessive water intake. Family member involvement in monitoring.
Question 2: Viva Voce Questions & Answers
Q: What are the criteria for diagnosing SIADH?
A: SIADH diagnosis requires five criteria. (1) Hypotonic hyponatremia with serum osmolality <280 mOsm/kg and sodium <135 mEq/L. (2) Urine osmolality >100 mOsm/kg (typically >300) despite plasma hypotonicity. (3) Urine sodium >40 mEq/L on normal dietary sodium intake. (4) Clinical euvolemia without orthostatic hypotension, edema, or ascites. (5) Normal thyroid, adrenal, cardiac, renal, and hepatic function. Additional supportive features include hypouricemia (<4 mg/dL). Also low BUN (<10 mg/dL). Fractional excretion of uric acid >12% supports diagnosis.
Q: Why do loop diuretics rarely cause hyponatremia while thiazides commonly do?
A: Thiazides block the Na-Cl cotransporter in the distal convoluted tubule. This is the nephron’s main diluting segment. This impairs maximum urinary dilution. Prevents free water excretion. Raises minimum urine osmolality. In contrast, loop diuretics block the Na-K-2Cl cotransporter. This occurs in the thick ascending limb of Henle’s loop. This is the primary concentrating segment. Loop diuretics therefore impair urinary concentration. Promote free water excretion. Protect against hyponatremia development. Despite causing sodium losses. This explains why severe diuretic-induced hyponatremia almost exclusively occurs with thiazides. Rather than furosemide or bumetanide.
Q: What is osmotic demyelination syndrome and how can it be prevented?
A: Osmotic demyelination syndrome (ODS) was previously called central pontine myelinolysis. Occurs when chronic hyponatremia corrects too rapidly. During chronic hyponatremia, brain cells adapt. Extrude organic osmolytes (glutamate, taurine, myo-inositol). Reduces cerebral edema. Rapid sodium correction causes osmotic stress. Cells cannot regenerate osmolytes quickly enough. Leads to white matter injury. Particularly affects pons, basal ganglia, and cerebellum. Symptoms appear 2-6 days post-correction. Include dysarthria, dysphagia, quadriparesis, behavioral changes. Can cause locked-in syndrome. Prevention requires strict adherence to hyponatremia correction rate limits. ≤10-12 mEq/L in 24 hours for most patients. ≤8 mEq/L for high-risk patients. High-risk criteria include sodium <120 mEq/L, alcoholism, cirrhosis, malnutrition, hypokalemia. If overcorrection occurs, rescue therapy with desmopressin and D5W. Re-lower sodium may reduce ODS risk.
Question 3: OSCE Station
Scenario:
You are the intern on night duty. A 55-year-old man with small cell lung cancer presents. Serum sodium is 122 mEq/L. He reports mild nausea but is oriented. BP 125/78, HR 76, no edema. Serum osmolality 262 mOsm/kg. Urine osmolality 485 mOsm/kg. Urine sodium 58 mEq/L. Senior resident asks you to explain diagnosis and outline management.
Expected Performance:
Diagnosis: Recognize SIADH from small cell lung cancer. This causes ectopic ADH production. Identify euvolemic hyponatremia with inappropriate urinary concentration. Classify as chronic (likely) asymptomatic-to-minimally symptomatic. Given mild presentation. Labs confirm SIADH criteria met.
Management Plan:
- Confirm no hypothyroidism or adrenal insufficiency
- Initiate fluid restriction <1000 mL/day
- Increase dietary sodium and protein
- Monitor sodium daily initially
- If inadequate response after 48 hours, consider second-line therapy
- Options include oral urea, salt tablets, or vaptans
- Avoid normal saline (would worsen hyponatremia)
- Target gradual correction ≤10-12 mEq/L per 24 hours
- Treat underlying malignancy (oncology consultation)
- Patient education about symptoms requiring emergency care
Question 4: MCQs (2 marks each)
Q1: A patient with sodium 118 mEq/L has seizures. Best initial treatment?
A) Normal saline 1 liter bolus
B) 3% hypertonic saline 100 mL bolus
C) Fluid restriction
D) Oral salt tablets
Answer: B – 3% hypertonic saline 100 mL bolus. Acute symptomatic hyponatremia with seizures requires immediate hypertonic saline. Target 4-6 mEq/L increase.
Q2: Which finding best differentiates SIADH from hypovolemic hyponatremia?
A) Urine osmolality >100 mOsm/kg
B) Serum sodium <135 mEq/L
C) Clinical euvolemia vs orthostatic hypotension
D) Urine sodium >40 mEq/L
Answer: C – Clinical euvolemia vs orthostatic hypotension. Volume status is key differentiator. SIADH shows euvolemia. Hypovolemic hyponatremia shows volume depletion signs.
Q3: Maximum safe correction rate in chronic hyponatremia?
A) 15 mEq/L in 24 hours
B) 10-12 mEq/L in 24 hours
C) 20 mEq/L in 24 hours
D) 5 mEq/L in 24 hours
Answer: B – 10-12 mEq/L in 24 hours for most patients. 8 mEq/L for high-risk patients. Prevents osmotic demyelination syndrome.
Question 5: Last-Minute Checklist
Before Your Exam:
- Memorize SIADH diagnostic criteria (5 points)
- Know correction rate limits (10-12 mEq/L per 24 hours)
- Remember high-risk ODS patients (alcoholism, cirrhosis, sodium <120)
- Understand why thiazides cause hyponatremia (block diluting segment)
- Know when to use 3% saline (acute symptomatic only)
- Remember ICD-10 code E87.1
- Understand Edelman equation (Na+K in numerator)
- Know urine sodium interpretation (<20 vs >40)
- Remember rescue therapy for overcorrection (desmopressin + D5W)
- Understand why normal saline worsens SIADH
Quick Mnemonics:
SALT for SIADH criteria:
- Serum osmolality <280
- Appropriate volume status (euvolemic)
- Low sodium <135
- Thirst not suppressed (inappropriate urine concentration)
Correction limits: “10 in 24, 18 in 48”
High-risk: “CHALK”
- Cirrhosis
- Hypokalemia
- Alcoholism
- Low sodium (<120)
- Kachexia/malnutrition
Conclusion
Hyponatremia in clinical practice remains the most common electrolyte disorder. Affects up to 30% of hospitalized patients. Understanding hyponatremia pathophysiology is crucial. Mastering diagnostic algorithms saves lives. Knowing types of hyponatremia guides treatment decisions. The hyponatremia workup must be systematic. Follow step-by-step protocols. Recognize SIADH as the most common euvolemic cause. Be vigilant about thiazide-induced hyponatremia. Follow hyponatremia treatment guidelines carefully. Use hypertonic saline for hyponatremia appropriately. Respect hyponatremia correction rate limits strictly. Document with proper hyponatremia ICD-10 codes.
Key Takeaways:
- Acute symptomatic cases require immediate 3% saline
- Chronic cases need gradual correction (≤10-12 mEq/L per 24 hours)
- Never use normal saline in SIADH
- Always stop offending medications
- Monitor sodium every 4-6 hours during active treatment
- Account for potassium in correction calculations
- Use rescue therapy if overcorrection occurs
Want to master more essential medical topics? Visit simplymbbs.com for evidence-based guides. Written by medical professionals for students and doctors. Subscribe to our newsletter for weekly updates. Get exam-style questions delivered to your inbox. Access quick reference guides for clinical practice. Join thousands of medical students worldwide. Learn complex concepts made simple. Stay updated with latest clinical guidelines. Prepare for MBBS exams confidently. Master medicine, one topic at a time.