Have you ever wondered why doctors order a Complete Blood Count Interpretation: Red Flags, Clinical Correlates & Exam Caselets test so frequently? This single blood test can unveil a remarkable story about your health, from detecting hidden infections to identifying life-threatening conditions like leukemia. For medical students preparing for MBBS exams, mastering CBC interpretation is not just an academic requirement—it’s a fundamental clinical skill that can save lives in emergency departments and outpatient clinics alike.
The Complete Blood Count Interpretation: Red Flags, Clinical Correlates & Exam Caselets serves as the cornerstone of diagnostic hematology, providing quantitative and qualitative information about red blood cells, white blood cells, and platelets. Whether you’re a final-year medical student anxiously preparing for clinical postings, a resident doctor managing emergency cases, or simply someone trying to understand your lab reports, this comprehensive guide demystifies every parameter, red flag, and clinical correlation you need to know. Understanding CBC parameters explained empowers you to recognize patterns that point toward specific pathologies, from nutritional deficiencies to hematologic malignancies.
What Is Complete Blood Count?
Definition from Standard Medical Literature
According to Harrison’s Principles of Internal Medicine and other authoritative hematology texts followed worldwide, a complete blood count interpretation is a comprehensive panel of blood tests that measures the cellular components of blood, including red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes), along with their associated parameters and indices.
The CBC interpretation encompasses both quantitative measurements (absolute counts) and qualitative assessments (morphological characteristics) that provide critical diagnostic information across virtually all medical specialties. Modern automated hematology analyzers have revolutionized CBC test report reading by providing rapid, precise measurements of multiple parameters simultaneously, though peripheral blood smear examination remains essential for morphological correlation.
Components of CBC
A standard complete blood count interpretation includes the following components:
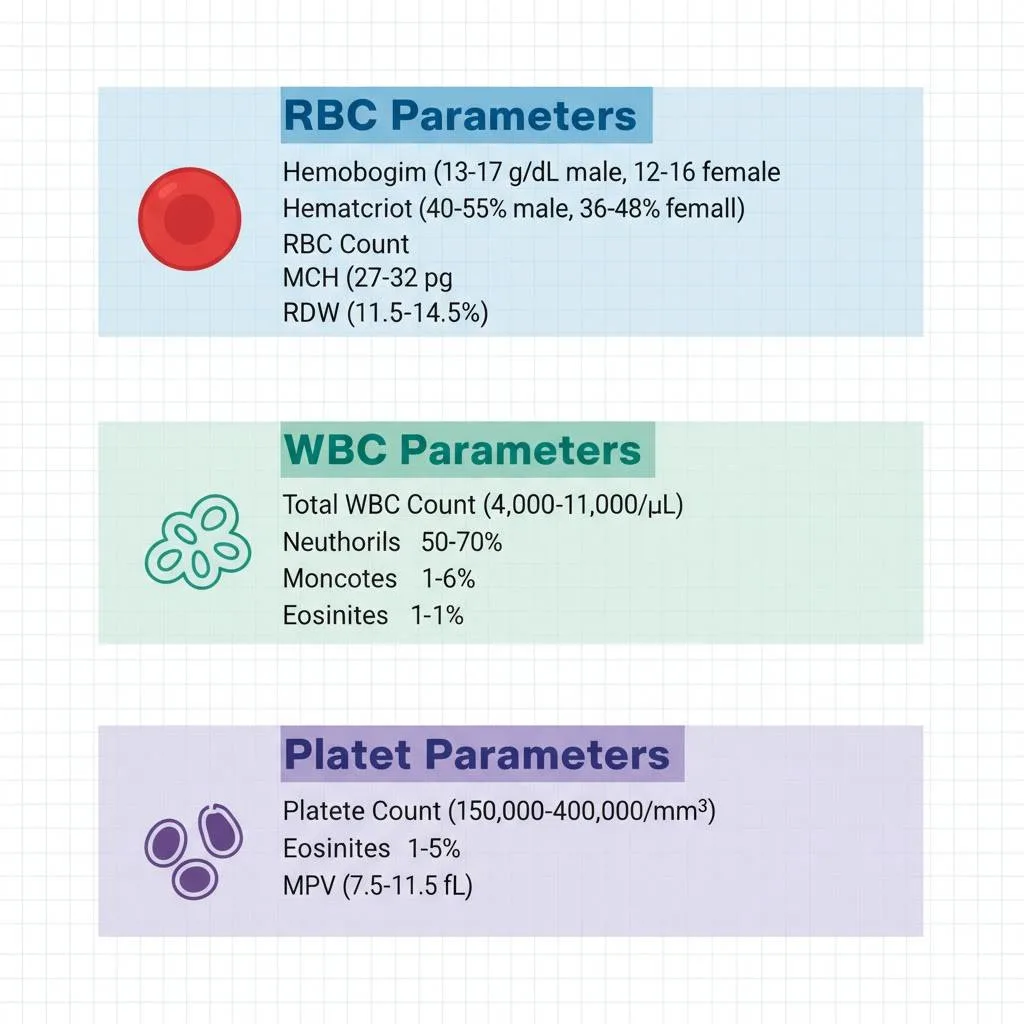
Red Blood Cell Parameters:
- Red blood cell count (RBC)
- Hemoglobin concentration (Hb/Hgb)
- Hematocrit (Hct)
- Mean corpuscular volume (MCV)
- Mean corpuscular hemoglobin (MCH)
- Mean corpuscular hemoglobin concentration (MCHC)
- Red cell distribution width (RDW)
White Blood Cell Parameters:
- Total white blood cell count (WBC)
- Differential count (neutrophils, lymphocytes, monocytes, eosinophils, basophils)
- Absolute counts for each WBC type
Platelet Parameters:
- Platelet count
- Mean platelet volume (MPV)
- Platelet distribution width (PDW)
Why CBC Matters
Clinical Significance for Students and Healthcare Professionals
The Complete Blood Count Interpretation: Red Flags, Clinical Correlates & Exam Caselets represents one of the most frequently ordered laboratory investigations in clinical medicine, and for compelling reasons. Understanding CBC normal ranges and their deviations forms the foundation for diagnosing hundreds of conditions, from simple iron deficiency to complex hematologic malignancies.
For MBBS students, mastering Blood Count interpretation offers several advantages:
- Provides a systematic approach to anemia diagnosis and classification
- Enables early detection of infections through WBC differential patterns
- Facilitates recognition of hematologic emergencies requiring immediate intervention
- Serves as a monitoring tool for chemotherapy, immunosuppressive therapy, and chronic diseases
- Forms the basis for understanding more complex hematology concepts
Real-Life Clinical Relevance
In emergency departments worldwide, complete blood count interpretation guides critical decision-making every day. A patient presenting with fatigue might have simple iron deficiency or life-threatening bone marrow failure. An elevated WBC count could indicate a bacterial infection requiring antibiotics or acute leukemia demanding urgent hematology consultation. Recognizing these patterns through systematic CBC test report reading directly impacts patient outcomes and prognosis.
Moreover, CBC parameters explained in the context of clinical presentations enhances diagnostic accuracy. A patient with anemia diagnosis and low MCV points toward iron deficiency or thalassemia, while high MCV suggests vitamin B12 or folate deficiency. These correlations between laboratory findings and clinical conditions form the essence of evidence-based medicine practiced globally.
Read More : Acute Kidney Injury (AKI): Clinical Classification, Urine Indices, and Management
Understanding RBC Parameters
Hemoglobin and Hematocrit
Hemoglobin (Hb/Hgb) measures the oxygen-carrying protein concentration in blood, expressed in grams per deciliter (g/dL). CBC normal ranges for hemoglobin vary by age and gender:
- Adult males: 13.0-17.0 g/dL
- Adult females: 11.5-15.5 g/dL
- Children: Age-dependent variations
Hematocrit (Hct) represents the percentage of blood volume occupied by red blood cells. Normal values include:
- Adult males: 40-55%
- Adult females: 36-48%
Low hemoglobin and hematocrit indicate anemia, while elevated values suggest polycythemia or dehydration. The hemoglobin vs hematocrit relationship typically follows a 3:1 ratio (Hb x 3 ≈ Hct), and significant deviations warrant investigation.
RBC Indices: The Diagnostic Keys
Mean Corpuscular Volume (MCV) quantifies the average red blood cell size, expressed in femtoliters (fL). CBC parameters explained for MCV classification:
- Microcytic: MCV < 80 fL (iron deficiency, thalassemia, chronic disease)
- Normocytic: MCV 80-100 fL (acute blood loss, hemolysis, chronic kidney disease)
- Macrocytic: MCV > 100 fL (B12/folate deficiency, alcoholism, liver disease)
Mean Corpuscular Hemoglobin (MCH) measures the average hemoglobin content per red blood cell (27-32 pg/cell). Low MCH produces hypochromic cells visible on peripheral smear, typically seen in iron deficiency.
Mean Corpuscular Hemoglobin Concentration (MCHC) indicates hemoglobin concentration within red blood cells (32-36 g/dL). Unlike MCH, MCHC accounts for cell volume and helps differentiate true iron deficiency from thalassemia.
Red Cell Distribution Width (RDW) quantifies variation in red blood cell size (normal: 11.5-14.5%). Elevated RDW indicates anisocytosis and helps distinguish:
- Iron deficiency (high RDW) from thalassemia trait (normal RDW)
- Mixed nutritional deficiencies causing dimorphic populations
Decoding WBC Differential
Total WBC Count and Clinical Correlates
The total white blood cell count ranges from 4,000-11,000 cells/µL in adults. CBC interpretation of WBC abnormalities includes:
Leukocytosis (elevated WBC) indicates:
- Bacterial infections
- Inflammatory conditions
- Stress response
- Leukemia or myeloproliferative disorders
- Corticosteroid therapy
Leukopenia (decreased WBC) suggests:
- Viral infections
- Bone marrow suppression
- Autoimmune conditions
- Chemotherapy effects
Differential Count: Pattern Recognition
CBC test report reading requires understanding absolute counts, not just percentages. A relative lymphocytosis might actually represent absolute neutropenia.
Normal Differential Ranges:
- Neutrophils (segmented): 50-70% (1,800-8,000/µL absolute)
- Band neutrophils: 0-5% (0-550/µL absolute)
- Lymphocytes: 20-40% (1,000-5,000/µL absolute)
- Monocytes: 1-6% (100-800/µL absolute)
- Eosinophils: 1-5% (50-500/µL absolute)
- Basophils: 0-1% (0-200/µL absolute)
Clinical Interpretation Patterns
Neutrophilia (increased neutrophils) most commonly indicates bacterial infection, but also occurs in metabolic emergencies like diabetic ketoacidosis, tissue necrosis, and inflammatory conditions.
Neutropenia (decreased neutrophils < 1,500/µL) carries infection risk, especially when severe (< 500/µL), requiring urgent evaluation and possible prophylactic antibiotics.
Lymphocytosis suggests viral infections (infectious mononucleosis, CMV), chronic lymphocytic leukemia, or pertussis.
Monocytosis appears in chronic infections (tuberculosis), inflammatory bowel disease, and recovery from bone marrow suppression.
Eosinophilia indicates parasitic infections, allergic reactions, drug reactions, or hypereosinophilic syndromes.
Platelet Indices Interpretation
Platelet Count and Disorders
CBC normal ranges for platelets span 150,000-400,000/mm³. Platelet count interpretation includes:
Thrombocytopenia (low platelets) classification:
- Mild: 100,000-150,000/mm³
- Moderate: 50,000-100,000/mm³
- Severe: < 50,000/mm³
- Critical: < 20,000/mm³ (spontaneous bleeding risk)
Thrombocytosis (elevated platelets) occurs in:
- Reactive conditions (infection, inflammation, iron deficiency)
- Primary thrombocythemia
- Myeloproliferative disorders
Mean Platelet Volume: The Underutilized Parameter
Mean Platelet Volume (MPV) measures average platelet size (7.5-11.5 fL) and provides diagnostic clues for thrombocytopenia etiology. CBC parameters explained for MPV interpretation:
High MPV (≥ 8.8 fL) with thrombocytopenia suggests:
- Increased platelet destruction (immune thrombocytopenic purpura)
- Peripheral consumption (disseminated intravascular coagulation)
- Increased turnover states
Low or Normal MPV with thrombocytopenia indicates:
- Decreased production (bone marrow failure)
- Aplastic anemia
- Chemotherapy effects
This distinction helps avoid unnecessary bone marrow biopsies, as MPV ≥ 8.8 fL has acceptable sensitivity and specificity for diagnosing destructive thrombocytopenia. The correlation between MPV findings and peripheral blood smear examination enhances diagnostic accuracy.
Read More : Acute Myocardial Infarction (MI): ECG Changes, Early Treatment, and Post-MI Care
Red Flags & Critical Values
Emergency Recognition in CBC Interpretation
Critical or panic values represent results so abnormal they constitute immediate health risks requiring urgent clinical action. Understanding these red flags separates competent from excellent clinicians.
Critical Values Requiring Immediate Notification
Red Blood Cell Critical Values:
- Hemoglobin < 7.0 g/dL or > 20 g/dL
- Hematocrit < 20% or > 60%
- Severe anemia with acute symptoms (chest pain, dyspnea, altered mental status)
White Blood Cell Critical Values:
- WBC < 2,000/µL (severe leukopenia, infection risk)
- WBC > 30,000/µL (potential leukemia or severe infection)
- Presence of blasts (immediate hematology consultation)
- Severe neutropenia < 500/µL (medical emergency)
Platelet Critical Values:
- Platelet count < 20,000/mm³ (spontaneous bleeding risk)
- Platelet count > 1,000,000/mm³ (thrombotic risk)
Red Flags in Specific Clinical Contexts
Pancytopenia (decreased RBC, WBC, and platelets) represents a hematologic emergency requiring immediate workup for:
- Aplastic anemia
- Bone marrow infiltration (leukemia, metastatic cancer)
- Severe megaloblastic anemia
- Overwhelming sepsis
Left Shift (increased band neutrophils and immature forms) indicates severe infection or bone marrow stress, particularly concerning when accompanied by toxic granulation or Döhle bodies.
Abnormal Cell Morphology flagged by analyzers demands peripheral smear review:
- Nucleated RBCs (NRBCs) suggest bone marrow stress, hemolysis, or infiltration
- Atypical lymphocytes indicate viral infections or lymphoproliferative disorders
- Schistocytes point toward microangiopathic hemolytic anemia
Clinical Correlates & Pathologies
Pattern-Based Diagnostic Approach
Complete Blood Count Interpretation: Red Flags, Clinical Correlates & Exam Caselets excellence requires recognizing patterns that point toward specific pathologies. This systematic approach transforms raw numbers into clinical diagnoses.
Anemia Classification and Correlates
Microcytic Hypochromic Anemia (MCV < 80 fL, Low MCH):
| Finding | Iron Deficiency | Thalassemia Trait | Chronic Disease |
|---|---|---|---|
| MCV | Very low (<70) | Mildly low (70-80) | Low-normal |
| RDW | High (>15%) | Normal | Normal-High |
| Serum Ferritin | Low | Normal-High | High |
| TIBC | High | Normal | Low |
| Peripheral Smear | Hypochromia, pencil cells | Target cells, basophilic stippling | Mild changes |
- Acute blood loss
- Hemolysis (check reticulocyte count, LDH, bilirubin)
- Early iron deficiency
- Chronic kidney disease (check creatinine)
- Mixed deficiencies
Macrocytic Anemia (MCV > 100 fL):
- Megaloblastic: B12/folate deficiency (hypersegmented neutrophils on smear)
- Non-megaloblastic: Alcoholism, liver disease, hypothyroidism, reticulocytosis
WBC Pattern Recognition
Neutrophilic Leukocytosis with Left Shift:
- Bacterial infections (pneumonia, abscess, sepsis)
- Inflammatory conditions
- Tissue necrosis (myocardial infarction, burns)
Lymphocytosis:
- Viral infections: Infectious mononucleosis, CMV, pertussis
- Chronic lymphocytic leukemia (CLL): Mature-appearing lymphocytes, often > 50,000/µL
- Acute lymphoblastic leukemia (ALL): Presence of lymphoblasts
Eosinophilia:
- Parasitic infections (particularly helminths)
- Allergic reactions and atopic conditions
- Drug reactions
- Hypereosinophilic syndrome
- Churg-Strauss syndrome
Thrombocytopenia Differential
High MPV Thrombocytopenia (Destructive):
- Immune thrombocytopenic purpura (ITP)
- Drug-induced thrombocytopenia
- Disseminated intravascular coagulation (DIC)
- Thrombotic thrombocytopenic purpura (TTP)
Low/Normal MPV Thrombocytopenia (Hypoproductive):
- Aplastic anemia
- Bone marrow infiltration
- Chemotherapy effects
- Megaloblastic anemia
Peripheral Smear Correlation
When to Request Peripheral Smear Review
Modern automated analysers flag abnormalities requiring morphological confirmation. CBC interpretation improves significantly when correlated with peripheral smear findings.
Indications for Peripheral Smear:
- Analyzer flags (blasts, NRBCs, atypical lymphocytes)
- Unexplained cytopenias
- Suspected hemolysis
- Evaluation of anemia with abnormal indices
- Suspected hematologic malignancy
Key Morphological Findings
Red Blood Cell Morphology:
- Hypochromia: Central pallor > 1/3 cell diameter (iron deficiency)
- Target cells: Thalassemia, liver disease, hemoglobin C disease
- Spherocytes: Hereditary spherocytosis, autoimmune hemolytic anemia
- Schistocytes: Microangiopathic hemolytic anemia, TTP, DIC
- Basophilic stippling: Lead poisoning, thalassemia
- Howell-Jolly bodies: Asplenia, severe hemolysis
White Blood Cell Morphology:
- Toxic granulation: Severe infection, sepsis
- Döhle bodies: Infection, burns, pregnancy
- Hypersegmented neutrophils: Megaloblastic anemia (>5% with ≥6 lobes)
- Atypical lymphocytes: Viral infections (EBV, CMV)
- Blasts: Acute leukemia (requires immediate hematology referral)
Common Interpretation Mistakes to Avoid
Pitfalls in CBC Analysis
Even experienced clinicians make errors in CBC test report reading that can lead to missed diagnoses or unnecessary investigations. Awareness of these pitfalls enhances diagnostic accuracy.
Mistake 1: Ignoring Clinical Context
Laboratory values must always be interpreted alongside clinical presentation. A hemoglobin of 10 g/dL might be life-threatening in acute hemorrhage but chronic and compensated in thalassemia trait.
Mistake 2: Relying on Percentages Instead of Absolute Counts
A WBC differential showing 80% lymphocytes appears abnormal, but if total WBC is 5,000/µL, the absolute lymphocyte count (4,000/µL) remains normal. Always calculate absolute values for accurate interpretation.
Mistake 3: Missing Dimorphic Blood Pictures
Patients with combined iron and B12 deficiency may have normal MCV, masking both deficiencies. High RDW alerts to this possibility, requiring both iron studies and B12/folate levels.
Mistake 4: Overlooking Reticulocyte Count
Anemia with low reticulocyte count indicates production failure, while high reticulocytes suggest hemolysis or hemorrhage. This distinction dramatically narrows differential diagnosis.
Mistake 5: Ignoring Temporal Changes
A platelet count of 90,000/mm³ may seem acceptable until you note it was 250,000/mm³ last week. Rapid declines warrant urgent investigation regardless of absolute values.
Mistake 6: Misinterpreting “Normal” Ranges
Reference ranges represent 95% of healthy populations, meaning 5% of normal individuals fall outside these limits. Borderline abnormalities require clinical correlation rather than automatic further testing.
Mistake 7: Neglecting Peripheral Smear Correlation
Automated analyzers have limitations in detecting certain abnormalities like malaria parasites, blasts in early leukemia, or specific morphological features. Smear review provides irreplaceable information.
Step-by-Step CBC Interpretation Guide
Systematic Approach to Complete Blood Count
Follow this structured method for comprehensive complete blood count interpretation:
Step 1: Verify Patient Information and Timing
Check patient identity, collection time, and any relevant clinical history or medications affecting results.
2: Assess Hemoglobin and Hematocrit
- Determine if anemia (low), polycythemia (high), or normal
- Compare to patient’s baseline if available
- Consider dehydration status affecting concentration
3: Evaluate RBC Indices
- Classify anemia by MCV (microcytic, normocytic, macrocytic)
- Check RDW for variation in cell size
- Calculate or verify hemoglobin vs hematocrit ratio
- Assess MCH and MCHC for colour characteristics
4: Examine Total and Differential WBC Count
- Determine if leukocytosis, leukopenia, or normal
- Calculate absolute counts for each cell type
- Identify predominant cell type elevation
- Note presence of immature forms (bands, blasts)
5: Review Platelet Count and Indices
- Classify as thrombocytopenia, thrombocytosis, or normal
- Check MPV to assess platelet production vs. destruction
- Correlate with bleeding/clotting history
6: Identify Critical Values and Red Flags
- Screen for panic values requiring immediate notification
- Look for pancytopenia or multiple cytopenias
- Check for analyser flags (blasts, NRBCs, atypical cells)
7: Synthesize Clinical Pattern
- Integrate CBC findings with clinical presentation
- Generate differential diagnosis
- Determine if peripheral smear needed
- Plan additional investigations based on pattern
Comparison: CBC vs Other Hematologic Tests
Understanding the Diagnostic Hierarchy
While CBC interpretation provides fundamental information, certain clinical scenarios require additional testing.
| Test | Primary Use | When to Order | Information Provided |
|---|---|---|---|
| Complete Blood Count | Screening and monitoring | Routine evaluation, anemia, infection, bleeding | Cell counts, indices, basic morphology |
| Peripheral Smear | Morphological assessment | Abnormal CBC, cytopenias, suspected malignancy | Detailed cell morphology, parasites |
| Reticulocyte Count | Bone marrow response | Anemia workup | RBC production assessment |
| Iron Studies | Iron deficiency evaluation | Microcytic anemia | Ferritin, TIBC, serum iron, transferrin saturation |
| Vitamin B12/Folate | Macrocytic anemia workup | MCV >100 fL | Nutritional deficiency assessment |
| Bone Marrow Biopsy | Definitive diagnosis | Unexplained cytopenias, suspected malignancy | Cellularity, architecture, malignancy detection |
| Flow Cytometry | Leukemia/lymphoma diagnosis | Suspected hematologic malignancy | Cell surface markers, clonality |
Read More : Pneumonia: Clinical Approach, Diagnosis & Management
Expert Insights & Evidence-Based Practice
Current Guidelines and Research
Recent literature emphasizes pattern-based complete blood count interpretation over isolated parameter analysis. A study analysing 21 diverse patient cases demonstrated that structured CBC interpretation, when contextualized with clinical and biochemical information, identifies serious underlying pathology that might otherwise be missed.
The diagnostic algorithm integrating red cell indices, platelet counts, and WBC differentials with clinical context improves diagnostic accuracy and guides timely intervention. Research shows that 77% of peripheral blood smear findings correlate with automated analyser results, validating the importance of combined interpretation approaches.
Regarding thrombocytopenia evaluation, evidence indicates that MPV ≥8.8 fL has acceptable sensitivity and specificity for diagnosing over-destructive thrombocytopenia, potentially avoiding invasive bone marrow examination. This finding has particular relevance for emergency assessment protocols and clinical decision-making.
For sepsis diagnosis, newer parameters like monocyte distribution width (MDW) represent promising red flags to identify patients requiring further clinical and laboratory evaluations. These advances demonstrate the evolving nature of CBC parameters explained in contemporary medicine.
Frequently Asked Questions (FAQs) About CBC Interpretation
Q : What is a complete blood count (CBC) test?
A : A complete blood count interpretation test measures the cellular components of blood, including red blood cells (RBCs), white blood cells (WBCs), and platelets, along with associated parameters like hemoglobin, hematocrit, and cell indices. It provides comprehensive information about overall health and helps diagnose various conditions.
Q : What are normal CBC values?
A : CBC normal ranges vary by age, gender, and laboratory, but typical adult values include: Hemoglobin 12-17 g/dL, WBC 4,000-11,000/µL, and Platelets 150,000-400,000/mm³. Always compare results to your laboratory’s specific reference ranges.
Q : What does low hemoglobin indicate?
A : Low hemoglobin indicates anemia, which can result from iron deficiency, vitamin B12/folate deficiency, chronic disease, bleeding, or bone marrow disorders. The MCV helps classify anemia type and guide further testing for anemia diagnosis.
Q : When should I worry about abnormal CBC results?
A : Critical values requiring immediate medical attention include hemoglobin < 7 g/dL, WBC < 2,000 or > 30,000/µL, platelets < 20,000/mm³, or presence of abnormal cells like blasts. Contact your healthcare provider promptly for any significantly abnormal results accompanied by symptoms.
Q : What is MCV and why does it matter?
A : MCV (mean corpuscular volume) measures average red blood cell size and helps classify anemia. Low MCV suggests iron deficiency or thalassemia, normal MCV indicates acute blood loss or chronic disease, and high MCV points to B12/folate deficiency or alcohol use.
Q : What does high white blood cell count mean?
A : Elevated WBC (leukocytosis) commonly indicates infection, inflammation, stress, or less commonly, leukemia. CBC interpretation requires examining the differential count to determine which specific cell type is elevated and clinical correlation for diagnosis.
Q : Can CBC detect cancer?
A : CBC test report reading can provide clues suggesting cancer, such as unexplained anemia, abnormal WBC patterns, thrombocytopenia, or presence of abnormal cells. However, definitive cancer diagnosis requires additional tests like bone marrow biopsy or flow cytometry.
Exam Question-Answer Section (University Pattern)
Long Case-Based Question (10 Marks)
Question: A 35-year-old woman presents with progressive fatigue, pallor, and glossitis for 3 months. Her CBC shows: Hb 7.2 g/dL, MCV 112 fL, WBC 3,200/µL with hypersegmented neutrophils, Platelets 98,000/mm³. Peripheral smear shows macro-ovalocytes.
a) Interpret the CBC findings (3 marks)
b) What is the most likely diagnosis? (2 marks)
c) What additional investigations would you order? (3 marks)
d) Outline the management approach (2 marks)
Model Answer:
a) CBC Interpretation (3 marks):
- Severe macrocytic anemia (Hb 7.2 g/dL with MCV 112 fL) – 1 mark
- Mild leukopenia with hypersegmented neutrophils suggesting megaloblastic process – 1 mark
- Thrombocytopenia indicating bone marrow involvement – pancytopenia pattern – 1 mark
b) Most Likely Diagnosis (2 marks):
Megaloblastic anemia secondary to vitamin B12 or folate deficiency – 2 marks
(Award 1 mark if either B12 or folate deficiency mentioned alone)
c) Additional Investigations (3 marks):
- Serum vitamin B12 and folate levels (confirmatory) – 1 mark
- Reticulocyte count (expected to be low), LDH (elevated), indirect bilirubin (elevated) – 1 mark
- Intrinsic factor antibodies, parietal cell antibodies if B12 deficient; anti-tissue transglutaminase if folate deficient – 1 mark
d) Management Approach (2 marks):
- If B12 deficiency: Intramuscular cyanocobalamin 1000 µg daily for 1 week, then weekly for 4 weeks, then monthly maintenance – 1 mark
- If folate deficiency: Oral folic acid 1-5 mg daily; address underlying cause; monitor CBC response – 1 mark
Short Answer Question (5 Marks)
Question: Explain the significance of MPV (mean platelet volume) in differentiating causes of thrombocytopenia.
Model Answer (Bullet Points):
-
Definition: MPV measures average platelet size, normal range 7.5-11.5 fL – 1 mark
-
High MPV (≥8.8 fL) with thrombocytopenia: Indicates peripheral platelet destruction with compensatory release of young, large platelets from bone marrow – 1 mark
-
Examples: ITP, DIC, TTP, drug-induced thrombocytopenia
-
-
Low or normal MPV with thrombocytopenia: Suggests decreased platelet production from bone marrow failure or hypoproduction – 1 mark
-
Examples: Aplastic anemia, chemotherapy, bone marrow infiltration
-
-
Clinical Utility: MPV ≥8.8 fL has acceptable sensitivity/specificity for diagnosing destructive thrombocytopenia, potentially avoiding invasive bone marrow biopsy – 1 mark
-
Limitations: Should be interpreted with clinical context, peripheral smear, and other CBC parameters; not used in isolation – 1 mark
MCQ-Based Caselet (2 Marks Each)
Case 1: A 28-year-old man presents with fever and sore throat. CBC shows WBC 15,000/µL with 60% atypical lymphocytes. Which investigation is most likely to confirm the diagnosis?
a) Blood culture
b) Heterophile antibody test (Monospot)
c) Bone marrow biopsy
d) Flow cytometry
Answer: b) Heterophile antibody test (Monospot) – suggests infectious mononucleosis
Case 2: A 55-year-old woman’s CBC shows: Hb 9.5 g/dL, MCV 68 fL, RDW 18%, platelets normal. Iron studies show low ferritin. Which finding on peripheral smear would you expect?
a) Target cells
b) Hypochromic microcytic RBCs with pencil cells
c) Spherocytes
d) Macro-ovalocytes
Answer: b) Hypochromic microcytic RBCs with pencil cells – classic for iron deficiency anemia
Case 3: A patient receiving chemotherapy has CBC showing: WBC 1,200/µL, absolute neutrophil count 400/µL. This patient is at highest risk for:
a) Bleeding complications
b) Severe bacterial infections
c) Anemia symptoms
d) Thrombotic events
Answer: b) Severe bacterial infections – severe neutropenia (<500/µL) dramatically increases infection risk
Viva Tips for CBC Interpretation
Common Viva Questions:
- Define anemia and its classification
- Differentiate between absolute and relative counts in WBC differential
- Explain the significance of left shift
- Describe critical values in CBC requiring immediate action
- Interpret a given CBC report with clinical correlation
Key Points to Remember:
- Always start with clinical presentation before interpreting labs
- Calculate absolute counts for WBC differential
- Use MCV as the starting point for anemia classification
- Mention the need for peripheral smear in appropriate scenarios
- Discuss electrolyte abnormalities when relevant to diagnosis
- Reference related conditions requiring emergency assessment protocols
Last-Minute Checklist for Exams
RBC Parameters Must-Know:
- Hemoglobin normal ranges (male vs female)
- MCV cutoffs: <80, 80-100, >100 fL
- RDW significance in iron deficiency vs thalassemia
- Hemoglobin vs hematocrit 3:1 ratio
WBC Differential Essentials:
- Normal WBC range: 4,000-11,000/µL
- Neutrophil absolute count: 1,800-8,000/µL
- Severe neutropenia definition: <500/µL
- Left shift indicates infection/inflammation
Platelet Key Points:
- Normal range: 150,000-400,000/mm³
- Critical low value: <20,000/mm³
- MPV cutoff for destructive thrombocytopenia: ≥8.8 fL
Critical Values to Memorize:
- Hb <7 or >20 g/dL
- WBC <2,000 or >30,000/µL
- Platelets <20,000/mm³
- Presence of blasts = urgent hematology consult
Conclusion
Mastering Complete Blood Count Interpretation: Red Flags, Clinical Correlates & Exam Caselets represents a fundamental milestone in medical education and clinical practice. This comprehensive guide has equipped you with systematic approaches to CBC interpretation, from understanding basic CBC parameters explained to recognizing life-threatening critical values requiring immediate intervention. The pattern-based diagnostic framework presented here transforms raw laboratory data into actionable clinical insights, whether you’re managing acute kidney injury, investigating anemia diagnosis, or responding to metabolic emergencies.
For MBBS students, consistent practice with CBC test report reading alongside clinical scenarios solidifies pattern recognition skills essential for both examinations and future clinical practice. Remember that laboratory values never exist in isolation—clinical context, patient history, and physical examination findings complete the diagnostic picture. The integration of peripheral smear correlation, critical value recognition, and understanding when additional testing is warranted distinguishes competent clinicians from exceptional ones.
Continue expanding your medical knowledge by exploring related topics on Simply MBBS, including our comprehensive guides on cardiac markers, electrolyte abnormalities, emergency assessment protocols, and allergic reactions. Subscribe to our newsletter at simplymbbs.com for regular updates on medical education topics, exam preparation strategies, and evidence-based clinical pearls that will enhance your journey from medical student to confident physician. Your commitment to understanding CBC normal ranges, red flags, and clinical correlates today builds the foundation for excellent patient care tomorrow.