Anaphylactic shock represents one of medicine’s most urgent emergencies, requiring immediate recognition and treatment to prevent death. This severe, systemic allergic reaction can progress from mild symptoms to life-threatening cardiovascular collapse within minutes. For medical students, healthcare professionals, and the general public, understanding anaphylactic shock can literally mean the difference between life and death.
Every year, anaphylaxis affects approximately 1 in 50 Americans, with food allergies being the leading cause in children and medications in adults. Despite its prevalence, many people remain unaware of the warning signs or proper emergency response. This comprehensive guide will equip you with essential knowledge about anaphylactic shock, from recognizing early symptoms to administering life-saving treatment.
Whether you’re preparing for MBBS exams, working in healthcare, or simply want to protect yourself and loved ones, this article provides evidence-based information that could save lives. We’ll explore the pathophysiology behind this dramatic immune response, identify common triggers, and outline the critical steps needed when seconds count.
What is Anaphylactic Shock?
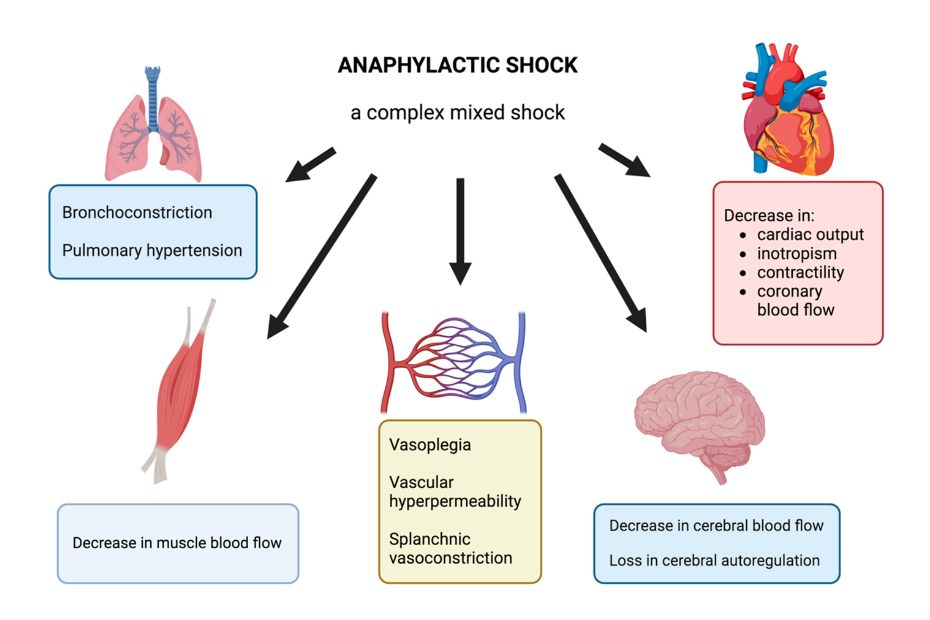
Anaphylactic shock occurs when the body’s immune system launches an overwhelming response to a previously encountered allergen, resulting in widespread inflammation and potentially fatal cardiovascular collapse. This medical emergency develops when anaphylaxis—a severe allergic reaction—progresses to involve multiple organ systems, particularly the cardiovascular system.
The pathophysiology involves immunoglobulin E (IgE) antibodies recognizing an allergen and triggering massive release of inflammatory mediators, primarily histamine, from mast cells and basophils. These chemicals cause widespread vasodilation, increased vascular permeability, and smooth muscle contraction throughout the body. Consequently, blood pressure drops dramatically while fluid shifts from blood vessels into tissues, creating the characteristic signs of anaphylactic shock.
Unlike milder allergic reactions that might only affect the skin or respiratory system, anaphylactic shock involves systemic circulatory failure. The combination of vasodilation and capillary leak leads to distributive shock, where adequate blood pressure cannot be maintained despite normal or increased heart rate. Without immediate intervention with epinephrine and supportive care, this condition can result in cardiac arrest and death within minutes.
Healthcare providers distinguish anaphylactic shock from other allergic reactions by the presence of hypotension (systolic blood pressure less than 90 mmHg in adults) along with signs of end-organ dysfunction. This critical distinction guides treatment decisions and emphasizes the urgent nature of the condition.
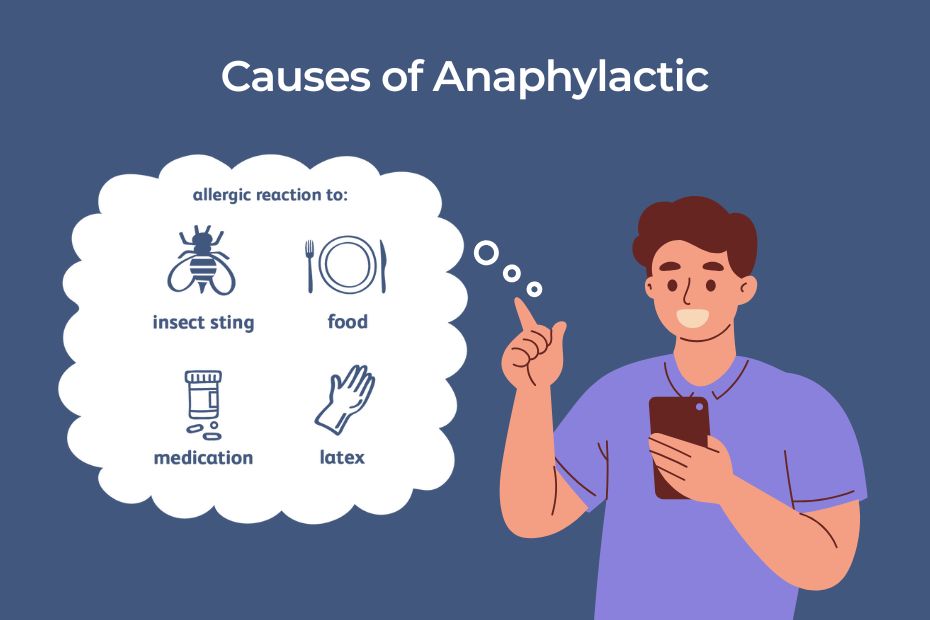
Common Causes and Triggers of Anaphylactic Shock
Understanding what triggers anaphylactic shock helps with both prevention and rapid recognition. The most common causes vary by age group, but certain allergens consistently rank among the top culprits.
1. Food Allergens
Food allergies represent the leading cause of anaphylaxis in children and young adults. The “Big 8” food allergens—milk, eggs, peanuts, tree nuts, soy, wheat, fish, and shellfish—account for approximately 90% of food-related anaphylactic reactions. Peanuts and tree nuts pose the highest risk for severe reactions, often causing symptoms within minutes of exposure.
Cross-contamination during food preparation frequently triggers unexpected reactions. Even trace amounts of allergens can provoke anaphylaxis in highly sensitive individuals. Restaurant meals, processed foods, and products manufactured in facilities that also process allergens carry particular risks.
2. Medications
Drug-induced anaphylaxis becomes more common with age, affecting adults more frequently than children. Antibiotics, particularly penicillin and related beta-lactams, cause the majority of medication-related anaphylactic reactions. Other high-risk medications include nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and certain anesthetics used during surgical procedures.
Radiocontrast media used in imaging studies can also trigger severe reactions, though newer formulations have reduced this risk. Healthcare providers must always obtain detailed allergy histories before administering any medications or contrast agents.
3. Insect Stings and Bites
Hymenoptera insects—including bees, wasps, hornets, and fire ants—cause approximately 100 deaths annually from anaphylaxis in the United States. These reactions typically occur in individuals who have been previously sensitized through earlier stings. The venom proteins act as potent allergens, triggering massive immune responses in susceptible people.
4. Less Common Triggers
Exercise-induced anaphylaxis represents a unique form where physical activity triggers symptoms, sometimes requiring co-factors like specific foods or medications consumed before exercise. Latex allergy, once common among healthcare workers, has decreased due to reduced latex glove usage but remains a concern in medical settings.
Idiopathic anaphylaxis occurs without identifiable triggers, making prevention challenging. These cases require careful evaluation and may benefit from prophylactic medications in some situations.
Also Read : RBC Development: Unleash the Medical Secrets
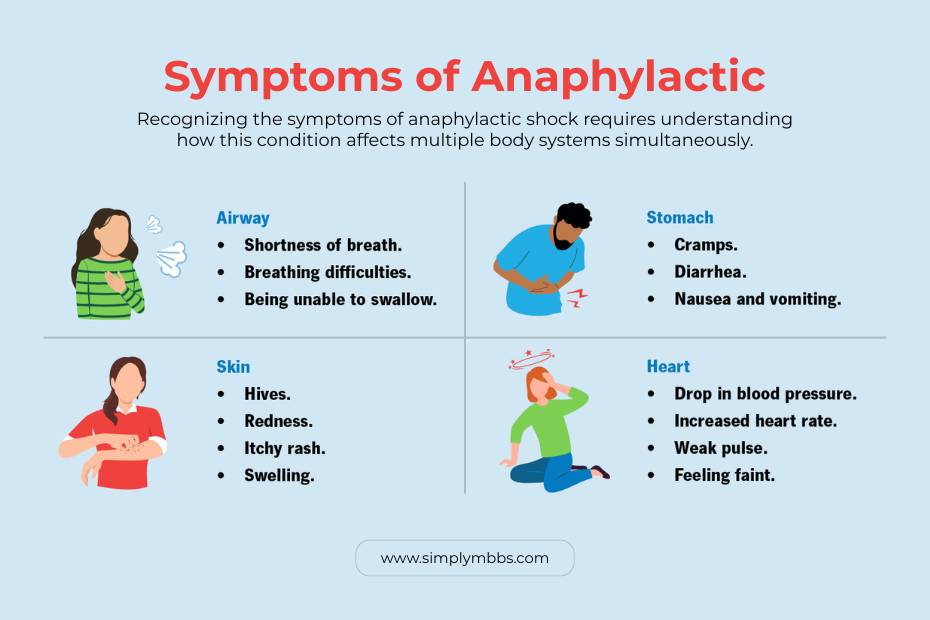
Signs and Symptoms of Anaphylactic Shock
Recognizing the symptoms of anaphylactic shock requires understanding how this condition affects multiple body systems simultaneously. Early recognition and intervention significantly improve outcomes, making symptom awareness crucial for everyone.
Early Warning Signs
Initial signs of anaphylactic shock often begin within minutes of allergen exposure, though onset can occasionally be delayed by hours. The skin typically shows the first changes, with generalized urticaria (hives), flushing, or intense itching affecting large body areas. However, importantly, skin symptoms may be absent in up to 20% of cases, particularly in very severe reactions.
Respiratory symptoms frequently accompany skin changes and include throat tightness, hoarseness, or difficulty swallowing. Patients often describe a sensation of their throat closing or tongue swelling. Wheezing, shortness of breath, and persistent coughing may develop as bronchospasm occurs.
Gastrointestinal symptoms such as nausea, vomiting, diarrhea, and severe abdominal cramping commonly occur, especially with food-triggered reactions. These symptoms result from smooth muscle contraction and increased intestinal secretions.
Cardiovascular Manifestations
The cardiovascular system bears the brunt of anaphylactic shock, with symptoms reflecting distributive shock physiology. Patients experience rapid heart rate (tachycardia) as the body attempts to compensate for falling blood pressure. However, blood pressure continues to drop due to widespread vasodilation and capillary leak.
Dizziness, lightheadedness, and feeling faint indicate inadequate brain perfusion. Patients may report feeling like they’re going to “pass out” or die. These symptoms reflect the body’s struggle to maintain adequate circulation to vital organs.
Severe Progressive Symptoms
As anaphylactic shock progresses, signs and symptoms of anaphylactic shock become more dramatic and life-threatening. Severe breathing difficulty develops as upper airway swelling combines with lower airway bronchospasm. Patients may make high-pitched sounds when breathing (stridor) or exhibit accessory muscle use.
Loss of consciousness occurs as blood pressure falls below levels needed to perfuse the brain adequately. Cardiac arrest represents the final common pathway if treatment is delayed. The combination of severe hypotension, hypoxemia, and metabolic acidosis creates a deadly cycle that becomes increasingly difficult to reverse.
Anaphylactic Shock Treatment: Immediate Life-Saving Interventions
Anaphylactic shock treatment follows established protocols that prioritize rapid reversal of the underlying pathophysiology. Success depends on immediate recognition and prompt administration of appropriate medications, with epinephrine serving as the cornerstone of therapy.
1. Emergency Epinephrine Administration
Epinephrine represents the only medication capable of reversing anaphylaxis and preventing progression to shock. This medication works by stimulating alpha and beta-adrenergic receptors, causing vasoconstriction to restore blood pressure and bronchodilation to improve breathing. Additionally, epinephrine stabilizes mast cells, preventing further mediator release.
The standard dose for adults is 0.3-0.5 mg of 1:1000 epinephrine given intramuscularly in the outer thigh. Children receive 0.01 mg/kg up to 0.3 mg maximum. Auto-injectors like EpiPen deliver pre-measured doses and should be used immediately when available. The injection should be given through clothing if necessary, as delay increases mortality risk.
Repeat doses may be needed every 5-15 minutes if symptoms persist or worsen. Healthcare providers should prepare for multiple injections, as severe reactions often require 2-3 doses for adequate response.
2. Immediate Emergency Response
Simultaneously with epinephrine administration, emergency medical services must be activated by calling 911. Even if symptoms appear to improve, patients require hospital evaluation due to the risk of biphasic reactions—where symptoms return hours after apparent recovery.
Position the patient lying flat with legs elevated unless breathing difficulty makes this impossible. This position helps maintain blood flow to vital organs. Remove or discontinue exposure to suspected triggers when possible.
3. Hospital-Based Treatment
Emergency department management includes intravenous fluid resuscitation to restore intravascular volume and support blood pressure. Large-bore IV access allows rapid fluid administration, typically with normal saline or lactated Ringer’s solution.
Supplemental oxygen addresses hypoxemia from respiratory involvement. Severe cases may require intubation and mechanical ventilation if upper airway swelling threatens complete obstruction.
Additional medications include H1 antihistamines (diphenhydramine) and H2 antihistamines (ranitidine or famotidine) to counteract histamine effects. Corticosteroids like methylprednisolone may prevent late-phase reactions, though they don’t help with acute symptoms.
Vasopressor medications such as dopamine or norepinephrine become necessary when epinephrine and fluids fail to restore adequate blood pressure. These medications require intensive care unit monitoring and titration.
Also Read : The Brachial Plexus: An Anatomical Overview
Anaphylactic Shock in Specific Populations
Different populations experience unique considerations regarding anaphylaxis recognition, treatment, and prevention strategies that healthcare providers must understand.
Pediatric Considerations
Children present additional challenges in anaphylaxis management due to their smaller size, different physiology, and communication limitations. Anaphylactic shock symptoms in children may be subtle initially, with behavioral changes like irritability, clinging behavior, or sudden lethargy serving as early warning signs.
Weight-based epinephrine dosing requires careful calculation, with most pediatric auto-injectors containing 0.15 mg for children weighing 15-30 kg and 0.3 mg for those over 30 kg. School settings require special protocols ensuring trained staff can recognize symptoms and administer emergency medications.
Food allergies predominate in pediatric anaphylaxis, making cafeteria safety and peer education crucial. Children often cannot articulate their symptoms clearly, making caregiver observation skills essential for early recognition.
Anaphylactic Shock in Dogs
While this guide focuses on human anaphylaxis, anaphylactic shock in dogs shares similar pathophysiology and requires veterinary emergency care. Common triggers include insect stings, vaccines, and certain foods. Symptoms include facial swelling, difficulty breathing, vomiting, and collapse.
Veterinary treatment follows similar principles with epinephrine, fluids, and supportive care. Pet owners should seek immediate veterinary attention for suspected anaphylaxis, as delays can be fatal.
Prevention Strategies and Long-Term Management
Preventing anaphylactic shock requires comprehensive approaches combining trigger avoidance, emergency preparedness, and sometimes medical therapy.
1. Allergen Identification and Avoidance
Formal allergy testing helps identify specific triggers through skin tests or blood-based assays measuring specific IgE antibodies. This testing guides avoidance strategies and helps predict reaction severity.
Food allergies require meticulous label reading, restaurant communication, and cross-contamination awareness. Support from registered dietitians helps ensure nutritional adequacy while avoiding allergens.
Drug allergies necessitate medical alert bracelets and clear communication with all healthcare providers. Electronic health records should prominently display allergy information to prevent accidental exposure during medical care.
2. Emergency Action Plans
All individuals with anaphylaxis risk should have written action plans outlining symptom recognition, medication administration, and emergency contact information. These plans require regular updates and review with healthcare providers.
Family members, teachers, and coworkers need training in recognizing symptoms and using auto-injectors. Practice sessions help ensure proper technique during actual emergencies when stress levels are high.
3. Carrying Emergency Medications
Prescription of two epinephrine auto-injectors ensures backup availability, as devices can malfunction or require multiple doses. Patients must carry these medications at all times, with additional units stored at home, work, and school.
Regular prescription renewals prevent expiration, as outdated epinephrine loses potency and may not provide adequate treatment. Most auto-injectors expire after 12-18 months.
Also Read : Knee Joint Anatomy: The Most Helpful Joint
Living with Anaphylaxis: Psychological and Social Aspects
The threat of potentially fatal reactions creates significant psychological burdens for patients and families affected by severe allergies. Anxiety, depression, and social isolation commonly develop, particularly among adolescents and young adults.
Managing Anxiety and Fear
Cognitive-behavioral therapy helps individuals develop coping strategies for managing allergy-related anxiety. Techniques include relaxation training, gradual exposure to previously avoided situations, and cognitive restructuring to address catastrophic thinking patterns.
Support groups connect individuals facing similar challenges, providing practical advice and emotional support. Online communities offer 24/7 access to peer support and expert guidance.
Creating Comprehensive Action Plans
Beyond emergency medication administration, action plans should address communication strategies, workplace accommodations, and travel considerations. Regular drills help maintain preparedness without creating excessive anxiety.
Schools require detailed management plans including staff training, medication storage, and emergency procedures. Federal laws protect students’ rights to carry emergency medications and receive appropriate accommodations.
Exam-Style Questions and Answers for Medical Students
Understanding anaphylactic shock requires mastery of both theoretical knowledge and practical application skills essential for MBBS examinations and clinical practice.
Common Exam Patterns
Medical school examinations frequently test anaphylaxis through case-based scenarios requiring rapid diagnosis and treatment planning. Students must demonstrate understanding of pathophysiology, symptom recognition, and emergency management protocols.
Multiple choice questions often focus on distinguishing anaphylaxis from other allergic reactions, appropriate medication dosing, and timing of interventions. Essay questions may explore prevention strategies, patient education, or complications of delayed treatment.
Practical examinations might simulate emergency scenarios where students must perform rapid assessment, medication administration, and communication with emergency services. These assessments evaluate both knowledge and clinical decision-making under pressure.
Frequently Asked Questions (FAQs)
#1 What is the fastest way to stop anaphylactic shock?
A : The fastest and most effective treatment is to immediately administer an epinephrine auto-injector (like an EpiPen) and then call 911. Epinephrine works within minutes to reverse severe symptoms, but medical supervision is still required.
#2 Can you survive anaphylactic shock without an EpiPen?
A : Survival is possible but highly unlikely, and the risk of death or severe complications is very high. Anaphylactic shock progresses rapidly, causing airway blockage and a dangerous drop in blood pressure. Immediate epinephrine is critical to survival.
#3 How long does it take to recover from anaphylactic shock?
A : Initial recovery from the most severe symptoms begins within minutes of receiving epinephrine. However, patients are typically observed in a hospital for at least 4-8 hours to monitor for a second wave of symptoms (biphasic reaction). Full recovery can take a few days.
#4 Can you develop anaphylaxis later in life?
A : Yes, it is possible to develop an allergy and the potential for anaphylaxis at any age, even to something you have been exposed to before without any issues. The immune system can change over time.
#5 What is the difference between anaphylaxis and anaphylactic shock?
A : Anaphylaxis is the severe, systemic allergic reaction itself. Anaphylactic shock is a component of anaphylaxis where the reaction causes a critical and life-threatening drop in blood pressure. All cases of anaphylactic shock are anaphylaxis, but not all anaphylaxis progresses to shock.