Every 34 seconds, someone in the United States dies from cardiovascular disease, with acute myocardial infarction being a leading cause. In India, cardiovascular disease strikes a decade earlier than in Western populations, with nearly 50% of all acute coronary syndrome cases occurring in men under 50 years of age. Understanding Acute Myocardial Infarction (MI), commonly known as a heart attack, is crucial for medical students, doctors, and the general public to recognize symptoms early, implement life-saving interventions, and reduce mortality rates.
What is Acute Myocardial Infarction?
Standard Medical Definition
Acute Myocardial Infarction (MI), or acute MI, refers to myocardial cell death (necrosis) caused by prolonged ischemia resulting from an acute interruption of coronary blood supply. According to the Universal Definition of Myocardial Infarction, diagnosis requires detection of elevated cardiac biomarkers (preferably cardiac troponin) with at least one value above the 99th percentile upper reference limit, along with evidence of acute myocardial ischemia manifesting as symptoms, new ischemic ECG changes, or imaging evidence of new loss of viable myocardium.
The condition represents a medical emergency where coronary artery occlusion, typically due to atherosclerotic plaque rupture and subsequent thrombus formation, leads to insufficient oxygen delivery to cardiac muscle tissue. Without prompt revascularization, irreversible myocardial damage occurs within 20-40 minutes of complete ischemia.
Why Understanding Acute Myocardial Infarction Matters
Global and Regional Impact
The burden of myocardial infarction extends across continents with varying patterns and outcomes. In the United States, 919,032 people died from cardiovascular disease in 2023, with one person dying every 34 seconds. The absolute prevalence of cardiovascular disease in India exceeds 54.6 million cases, representing more than 60% higher prevalence than the United States despite India’s higher population density.
India faces a unique challenge where CVD death rates increased from 155.7 to 209.1 per 100,000 between 1990 and 2016, primarily driven by population aging. The age-standardized CVD death rate of 272 per 100,000 in India surpasses the global average of 235 per 100,000, indicating a disproportionately higher disease burden. Between 2025 and 2050, crude cardiovascular mortality in Asia is projected to rise 91.2% despite a 23.0% decrease in age-standardized rates.
For MBBS students and doctors, mastering Acute Myocardial Infarction diagnosis and management directly translates to saving lives in emergency departments and intensive care units. For the general public, recognizing early warning signs enables timely medical attention, which is critical since survival to hospital discharge for out-of-hospital cardiac arrests remains only 10.2% in the United States.
Types of Acute Myocardial Infarction
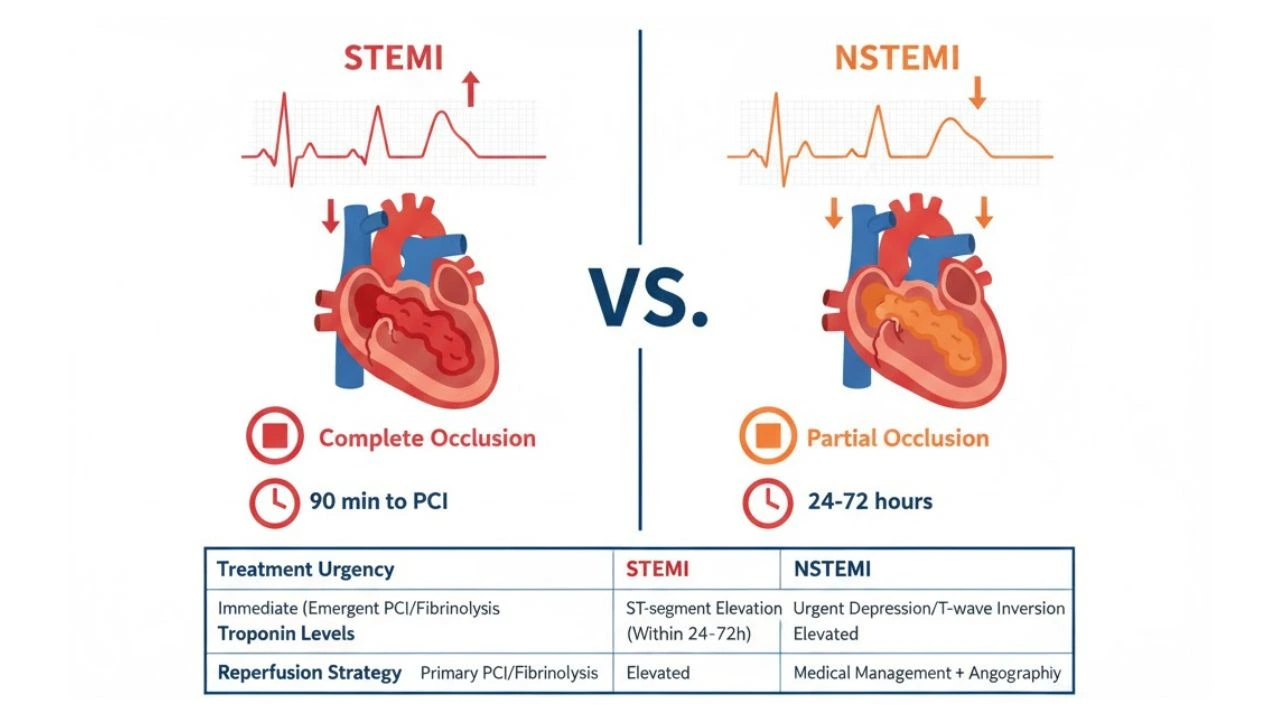
Acute myocardial infarction classification primarily divides into two critical categories based on electrocardiographic findings and pathophysiology:
STEMI vs NSTEMI Comparison
| Feature | STEMI (ST-Elevation MI) | NSTEMI (Non-ST-Elevation MI) |
|---|---|---|
| ECG Finding | ST-segment elevation ≥1mm in contiguous leads | ST-segment depression or T-wave inversion |
| Pathophysiology | Complete coronary artery occlusion | Partial occlusion or intermittent flow |
| Troponin | Markedly elevated | Elevated but variable |
| Treatment Priority | Immediate reperfusion (PCI <90 min) | Risk stratification, medical management |
| Thrombus Type | Occlusive, platelet-rich | Non-occlusive or dynamic |
| Mortality Risk | Higher acute phase mortality | Lower initial but comparable long-term risk |
STEMI represents the more urgent scenario requiring immediate reperfusion therapy within 90-120 minutes of first medical contact to prevent extensive myocardial necrosis. NSTEMI allows for a more measured approach with risk stratification and early invasive management within 24-72 hours depending on risk factors.
How MI Happens: Pathophysiology
Step-by-Step Process
Understanding how heart attack develops requires examining the cascade from atherosclerotic plaque formation to myocardial cell death:
Step 1: Atherosclerotic Plaque Development
Chronic exposure to cardiovascular risk factors (hypertension, diabetes, dyslipidemia, smoking) causes endothelial dysfunction in coronary arteries. Lipid accumulation within the arterial wall forms atherosclerotic plaques over years to decades, progressively narrowing the vessel lumen.
Step 2: Plaque Rupture or Erosion
Vulnerable plaques with thin fibrous caps and large lipid cores become unstable due to inflammation, mechanical stress, or hemodynamic forces. Rupture exposes thrombogenic material to circulating blood, triggering platelet activation and aggregation.
Step 3: Thrombus Formation
Activated platelets release vasoactive substances and initiate the coagulation cascade, forming an occlusive or partially occlusive thrombus. In STEMI, the thrombus completely blocks coronary blood flow, while in NSTEMI, partial obstruction or intermittent occlusion occurs.
Step 4: Myocardial Ischemia
Reduced coronary perfusion creates a supply-demand mismatch where oxygen delivery fails to meet myocardial metabolic requirements. Ischemic myocardium shifts from aerobic to anaerobic metabolism, depleting ATP stores and accumulating toxic metabolites.
Step 5: Myocardial Necrosis
Without reperfusion, irreversible cell death begins within 20-40 minutes of complete occlusion. Necrosis progresses from the subendocardium (inner layer) toward the subepicardium (outer layer) in a “wave-front phenomenon”. Myocyte death releases cardiac-specific proteins including troponin into circulation, enabling biochemical diagnosis.
Step 6: Complications and Remodeling
Following acute injury, the heart undergoes structural and functional remodeling that can lead to heart failure complications, arrhythmias, or mechanical complications depending on infarct size and location.
ECG Changes in Acute Myocardial Infarction (MI)
Electrocardiography remains the cornerstone diagnostic tool for acute myocardial infarction, enabling rapid differentiation between STEMI and NSTEMI and guiding immediate treatment decisions.
ST Elevation Criteria
Accurate identification of STEMI ECG changes requires understanding specific measurement thresholds and anatomical lead groupings:
| Lead Location | ST-Elevation Threshold | Clinical Significance |
|---|---|---|
| Limb Leads (I, II, III, aVL, aVF) | ≥1 mm (0.1 mV) in two contiguous leads | Inferior, lateral, or high lateral MI |
| V1-V6 (except V2-V3) | ≥1 mm in two contiguous leads | Anterolateral MI |
| V2-V3 (Men <40 years) | ≥2.5 mm | Anterior MI (age-adjusted) |
| V2-V3 (Men ≥40 years) | ≥2.0 mm | Anterior MI |
| V2-V3 (Women, any age) | ≥1.5 mm | Anterior MI (gender-adjusted) |
ST-segment elevation must be measured at the J-point, which is the junction where the QRS complex ends and the ST segment begins, assessed 0.04 seconds after the J-point. Contiguous leads refer to anatomically neighboring leads reflecting the same myocardial territory, such as V1-V6 (anterior), II/III/aVF (inferior), and I/aVL (lateral).
MI ECG Leads Explained
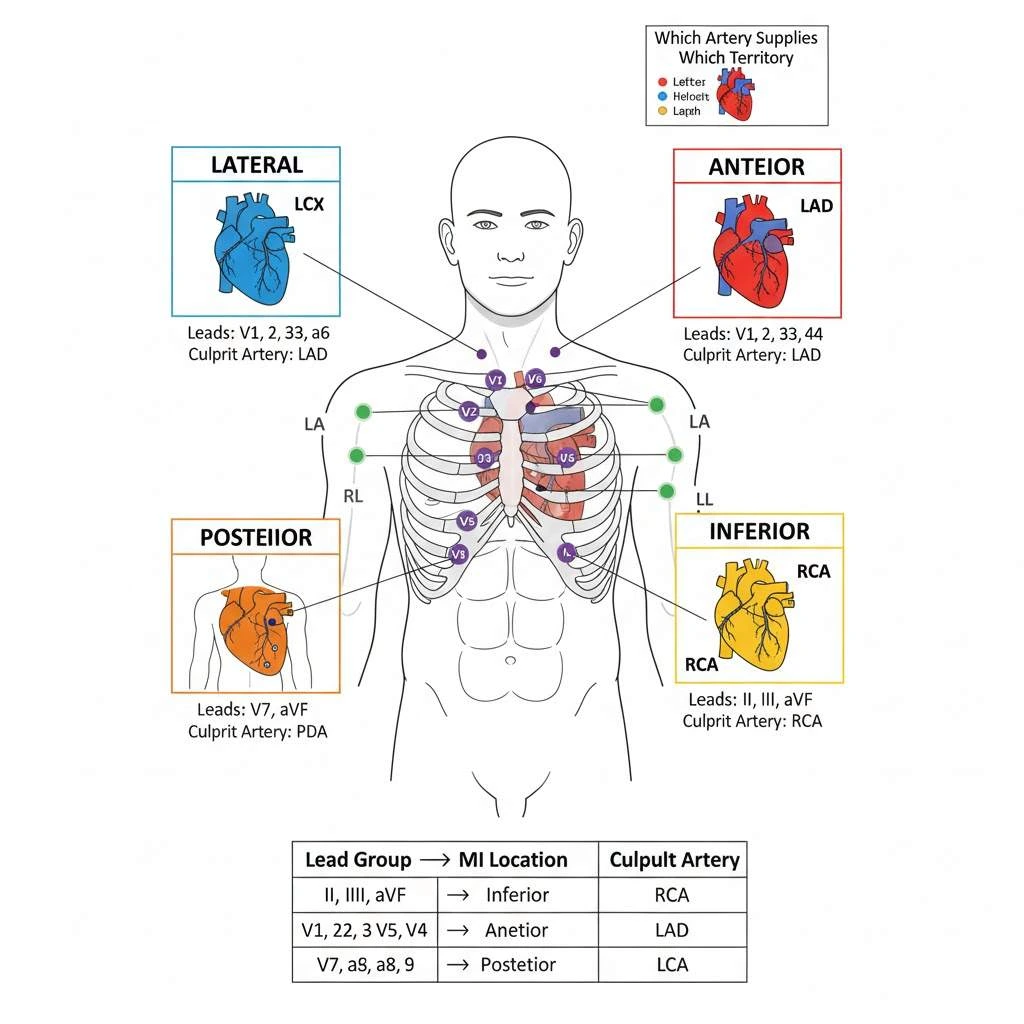
Understanding which MI ECG leads correspond to specific coronary territories guides diagnosis and treatment planning:
Inferior MI (II, III, aVF)
Right coronary artery (RCA) or left circumflex (LCx) occlusion causes ST elevation in inferior leads. Lead III elevation > lead II suggests RCA involvement, while lead I and aVL reciprocal depression confirms diagnosis.
Anterior MI (V1-V4)
Left anterior descending (LAD) artery occlusion produces ST elevation in anterior precordial leads. Proximal LAD occlusion affects leads V1-V6, I, and aVL, indicating extensive myocardium at risk requiring urgent intervention.
Lateral MI (I, aVL, V5-V6)
Left circumflex artery or diagonal branch occlusion causes ST elevation in lateral leads. Isolated lateral MI may present with subtle ECG changes requiring careful ECG interpretation skills.
Posterior MI (V7-V9)
Posterior wall infarction manifests as ST depression in leads V1-V3 with tall R waves (mirror image of posterior ST elevation). True posterior leads (V7-V9) placed on the posterior chest wall demonstrate diagnostic ST elevation.
Reciprocal ST Depression
Reciprocal ST depression represents ST-segment depression in leads electrically opposite to the infarct zone. This finding increases diagnostic specificity for STEMI by confirming that ST elevation results from acute coronary occlusion rather than benign early repolarization or pericarditis. Inferior MI typically shows reciprocal changes in leads I and aVL, while anterior MI may demonstrate reciprocal depression in inferior leads.
NSTEMI ECG Changes
Unlike STEMI’s distinctive elevation patterns, NSTEMI ECG changes present more subtly:
ST-Segment Depression
Horizontal or downsloping ST depression ≥0.5 mm in at least two anatomically contiguous leads indicates subendocardial ischemia. This pattern suggests partial coronary occlusion or severe stenosis with preserved epicardial perfusion.
T-Wave Inversion
Deep symmetric T-wave inversion ≥1 mm in leads with prominent R-waves (R/S ratio >1) indicates myocardial ischemia. Wellens’ syndrome, characterized by biphasic or deeply inverted T-waves in V2-V4, warns of critical LAD stenosis requiring urgent intervention.
Dynamic Changes
Serial ECG monitoring reveals evolving patterns in 15.7% of NSTEMI patients during transport. Transient ST-segment shifts, pseudonormalization of inverted T-waves, or development of pathological Q-waves help differentiate acute events from chronic changes.
Diagnosis: Cardiac Troponin
High-Sensitivity Troponin Algorithm
Cardiac troponin measurement represents the gold standard biomarker for Acute myocardial infarction diagnosis. High-sensitivity assays detect troponin elevations in up to 50% of healthy individuals, necessitating specific diagnostic algorithms to differentiate acute MI from chronic elevation or other causes of myocardial injury.
0/1-Hour Algorithm
The European Society of Cardiology recommends a high-sensitivity troponin algorithm using serial measurements at presentation (0 hours) and after 1 hour:
Rule-Out Criteria:
- hs-cTnT <5 ng/L at presentation AND <3 ng/L change at 1 hour
- hs-cTnI <4-6 ng/L at presentation AND minimal delta change
- Negative predictive value exceeds 99.5%
Rule-In Criteria:
- hs-cTnT ≥52 ng/L at presentation OR ≥5 ng/L rise at 1 hour
- Positive predictive value ranges 70-75%
- Requires clinical context and ECG correlation
0/2-Hour Alternative
When 1-hour sampling proves logistically challenging, a 0/2-hour algorithm using point-of-care hs-cTnI enables safe and efficient risk assessment. Studies demonstrate comparable diagnostic accuracy with 2-hour protocols, facilitating implementation in busy emergency departments.
Clinical Context Integration
Troponin elevation alone does not confirm acute MI; integration with clinical presentation, ECG findings, and imaging remains essential. Non-ischemic causes of troponin elevation include myocarditis, takotsubo cardiomyopathy, pulmonary embolism, chronic kidney disease, sepsis, and heart failure.
Immediate Management of Acute Myocardial Infarction
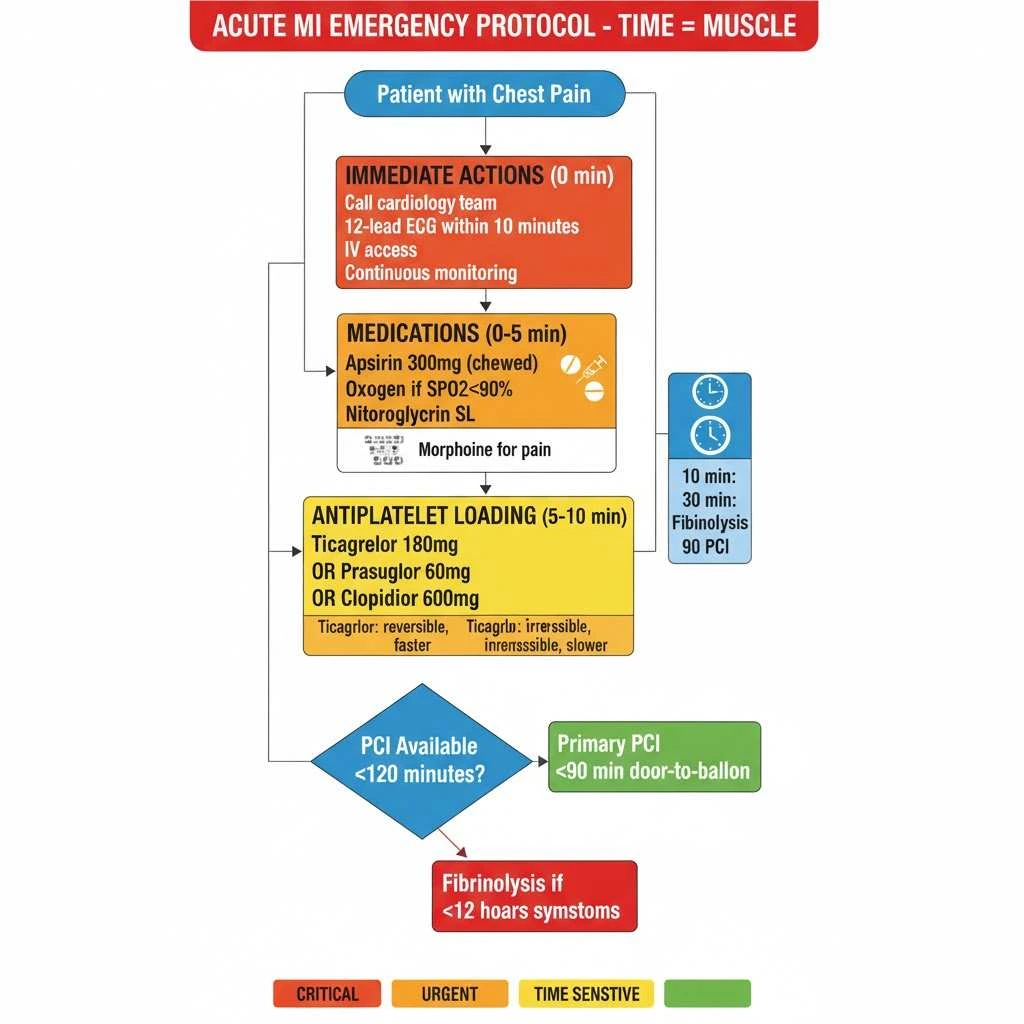
Time-sensitive interventions determine outcomes in acute myocardial infarction, with each 30-minute delay in reperfusion associated with increased mortality.
Aspirin Loading Dose in MI
Aspirin forms the cornerstone of antiplatelet therapy, providing immediate irreversible cyclooxygenase-1 inhibition to prevent thrombus propagation. The aspirin loading dose in MI consists of 162-325 mg (typically 300-325 mg) administered immediately upon AMI suspicion, preferably as chewable formulation for rapid buccal absorption.
Following the loading dose, maintenance therapy continues with 75-100 mg daily indefinitely in the absence of contraindications. This simple intervention reduces mortality by approximately 23% and should not be delayed for confirmatory testing.
Dual Antiplatelet Therapy for MI
Dual antiplatelet therapy combining aspirin with a P2Y12 inhibitor significantly reduces cardiovascular death, myocardial infarction, and stroke compared to aspirin monotherapy.
P2Y12 Inhibitors Options:
Clopidogrel
- Loading dose: 300-600 mg (600 mg preferred for primary PCI)
- Maintenance: 75 mg daily
- Onset: 2-6 hours (loading dose dependent)
- Considerations: Prodrug requiring CYP2C19 activation; genetic polymorphisms affect efficacy
Prasugrel
- Loading dose: 60 mg
- Maintenance: 10 mg daily (5 mg if <60 kg)
- Onset: 30 minutes
- Contraindications: Prior stroke/TIA, age >75 years, weight <60 kg (relative)
Ticagrelor
- Loading dose: 180 mg
- Maintenance: 90 mg twice daily
- Onset: 30 minutes
- Advantages: Reversible binding, no prodrug activation, dyspnea side effect in 10-15%
Dual Antiplatelet Duration After MI
Short-term (Acute Phase)
All STEMI and NSTEMI patients receive dual antiplatelet therapy for MI during hospitalization and for minimum 12 months post-event. This standard duration derives from landmark CURE and CLARITY-TIMI 28 trials demonstrating 20% relative risk reduction in major adverse cardiovascular events.
Extended Therapy (>12 months)
Selected high-risk patients benefit from extended DAPT beyond 12 months. The PEGASUS-TIMI 54 trial established that ticagrelor 60 mg twice daily combined with aspirin reduced cardiovascular death (HR 0.71), MI (HR 0.83), and all-cause death (HR 0.80) when continued 1-3 years post-MI, albeit with increased major bleeding risk (HR 2.36).
2025 ACC/AHA Guidelines
Current recommendations individualize dual antiplatelet duration after MI based on ischemic versus bleeding risk assessment. High ischemic risk (recurrent MI, multivessel disease, diabetes, chronic kidney disease) favours extended therapy, while high bleeding risk (prior bleeding, oral anticoagulation, advanced age) suggests shorter duration.
Long-Term Care After Acute Myocardial Infarction
Comprehensive secondary prevention transforms post-MI prognosis, with adherence to multiple guideline recommendations reducing long-term mortality by 39-43%.
Post-MI Care Plan
Medical Therapy Optimization
Lifelong medications form the foundation of post-MI care plan strategies:
- Antiplatelet therapy: Aspirin 75-100 mg daily indefinitely; P2Y12 inhibitor duration per risk assessment
- Beta-blockers: Metoprolol, carvedilol, or bisoprolol reduce mortality and recurrent MI
- ACE inhibitors/ARBs: Mandatory for anterior MI, LVEF <40%, diabetes, or hypertension
- Statins: High-intensity therapy (atorvastatin 80 mg or rosuvastatin 40 mg) targeting LDL <70 mg/dL
- Mineralocorticoid receptor antagonists: Eplerenone or spironolactone for LVEF ≤40%
Risk Factor Control
Target blood pressure <130/80 mmHg, HbA1c <7% for diabetes, and LDL cholesterol <70 mg/dL (optimally <55 mg/dL for very high-risk patients). Management of electrolyte imbalances like hyponatremia prevents arrhythmias and complications.
Lifestyle Changes After Heart Attack
Evidence-based lifestyle changes after heart attack provide comparable benefits to pharmacological interventions:
Smoking Cessation
Complete tobacco abstinence represents the single most effective secondary prevention measure, reducing mortality by 30-40%. Nicotine replacement therapy, varenicline, or bupropion combined with counseling achieves highest quit rates.
Mediterranean Diet
Adherence to Mediterranean-style or DASH eating patterns reduces cardiovascular events by 28%. Emphasize fruits, vegetables, whole grains, legumes, nuts, olive oil, and fatty fish while limiting red meat, processed foods, and saturated fats.
Physical Activity
Regular exercise 20-30 minutes daily to the point of slight breathlessness improves exercise capacity, reduces symptoms, and lowers mortality. Start gradually post-MI, progressing from comfortable levels toward moderate-intensity aerobic activity (50-70% maximum heart rate) 5 days weekly.
Weight Management
Target BMI 18.5-24.9 kg/m² and waist circumference <94 cm (men) or <80 cm (women). Each 5 kg weight loss in overweight individuals improves cardiovascular risk profile.
Alcohol Limitation
Restrict consumption to ≤1 drink daily for women, ≤2 drinks daily for men. Excessive alcohol increases blood pressure, triglycerides, and arrhythmia risk.
Cardiac Rehabilitation After Acute Myocardial Infarction
Cardiac rehabilitation represents a comprehensive, multidisciplinary intervention combining supervised exercise, education, counseling, and behavioral modification.
Core Components (2024 AHA Guidelines)
The American Heart Association updated cardiac rehabilitation standards in October 2024, emphasizing patient assessment, nutritional counseling, weight management, blood pressure/lipid management, tobacco cessation, psychosocial management, and physical activity counseling.
Exercise Prescription
Structured programs begin with baseline cardiopulmonary exercise testing to determine functional capacity and prescribe individualized exercise intensity. Progressive protocols target 90 MET-minutes accumulated during in-hospital phase, advancing to 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity weekly during outpatient phase.
In-Hospital Phase (Step 1-4)
Early mobilization begins 8-12 hours post-MI or revascularization for stable patients without complications. Gradual progression from bedside cycle ergometry to ambulation uses Borg Scale ratings of perceived exertion (target 9-10, corresponding to 2 METs), with twice-daily sessions until discharge.
Outpatient Phase (Phase II)
Supervised sessions 2-3 times weekly for 12 weeks provide monitored exercise, risk factor education, and psychosocial support. This phase demonstrates strongest evidence for mortality reduction (20-30% relative risk reduction) and improved quality of life.
Maintenance Phase (Phase III)
Long-term adherence to physical activity and healthy behaviors sustains benefits beyond formal rehabilitation. Telemonitoring and hybrid programs improve access for rural patients or those facing transportation barriers.
Barriers and Solutions
Despite proven benefits, only 20-30% of eligible MI patients participate in cardiac rehabilitation after MI programs. Addressing barriers through automatic referrals, insurance coverage expansion, flexible scheduling, and home-based alternatives improves utilization rates.
Common Mistakes to Avoid
Delaying Aspirin Administration
Never wait for troponin results or ECG confirmation before administering aspirin when acute MI is suspected. Every minute counts, and aspirin provides immediate antiplatelet effects without significant contraindications (except active GI bleeding).
Misinterpreting ECG Mimics
ST elevation occurs in conditions beyond coronary occlusion, including left ventricular hypertrophy, hyperkalemia, early repolarization, and pericarditis. Always correlate ECG findings with clinical presentation and serial troponin measurements before committing to reperfusion therapy.
Premature DAPT Discontinuation
Stopping P2Y12 inhibitors before 12 months dramatically increases stent thrombosis and recurrent MI risk. Address bleeding concerns through proton pump inhibitor co-prescription rather than discontinuing essential antiplatelet therapy.
Neglecting Cardiac Rehabilitation Referral
Automatic enrollment at hospital discharge dramatically improves cardiac rehabilitation participation rates. Similar to respiratory complications similar to pneumonia requiring comprehensive management, post-MI care necessitates structured rehabilitation programs.
Inadequate Secondary Prevention Education
Patients often leave hospital without clear understanding of medication purposes, lifestyle modifications, or warning signs requiring immediate attention. Structured discharge planning and follow-up within 7-14 days reinforces adherence.
Failing to Address Psychosocial Factors
Depression affects 20-30% of MI survivors and independently predicts mortality and non-adherence. Routine screening and mental health referrals constitute essential components of comprehensive recovery.
Frequently Asked Questions (FAQs)
Q : What is the difference between STEMI and NSTEMI?
A : STEMI shows ST-segment elevation ≥1 mm in contiguous ECG leads, indicating complete coronary occlusion requiring immediate reperfusion within 90 minutes. NSTEMI presents with ST depression or T-wave changes from partial occlusion, managed with early invasive strategy within 24-72 hours based on risk stratification.
Q : How long should dual antiplatelet therapy continue after MI?
A : Standard dual antiplatelet therapy duration after MI extends minimum 12 months for all patients. High ischemic risk patients may benefit from extended therapy up to 36 months using ticagrelor 60 mg twice daily, while high bleeding risk patients might shorten duration to 6 months with careful monitoring.
Q : What troponin level confirms myocardial infarction?
A : Diagnosis requires cardiac troponin elevation above the 99th percentile upper reference limit (typically 14-40 ng/L for hs-cTnT, 4-10 ng/L for hs-cTnI depending on assay) plus clinical evidence of acute ischemia. Absolute values matter less than dynamic changes and clinical context integration.
Q : Can you have a heart attack with normal ECG?
A : Yes, approximately 1-6% of acute MI patients present with normal or non-diagnostic initial ECGs. Serial ECGs every 15-30 minutes and troponin measurements at 0 and 1-2 hours identify these cases requiring emergency ABCDE approach assessment.
Q : When is thrombolysis preferred over primary PCI for STEMI?
A : Fibrinolytic therapy becomes preferred when anticipated door-to-balloon time exceeds 120 minutes and symptoms duration remains <12 hours. Rural patients without PCI access within 90-120 minutes benefit from immediate thrombolysis followed by transfer for angiography within 2-24 hours (pharmaco-invasive strategy).
Q : What loading doses should be given immediately in acute MI?
A : Aspirin loading dose in MI consists of 162-325 mg (preferably 300-325 mg chewed). Add P2Y12 inhibitor loading: clopidogrel 600 mg, prasugrel 60 mg, or ticagrelor 180 mg depending on clinical scenario and planned reperfusion strategy.
Exam Questions & Answers (University Pattern)
Question 1: Long Essay Question (20 Marks)
Q: A 55-year-old male presents to the emergency department with severe crushing chest pain radiating to the left arm for the past 2 hours. His ECG shows ST-segment elevation in leads II, III, and aVF with reciprocal depression in leads I and aVL. Discuss the diagnosis, pathophysiology, immediate management, and long-term secondary prevention strategies for this patient.
Model Answer (20 Marks Allocation):
A) Diagnosis (3 marks)
- Acute ST-Elevation Myocardial Infarction (STEMI) – inferior wall location
- ECG criteria met: ST elevation ≥1 mm in two contiguous inferior leads (II, III, aVF)
- Reciprocal ST depression in lateral leads (I, aVL) increases diagnostic specificity
B) Pathophysiology (4 marks)
- Right coronary artery (RCA) or left circumflex occlusion causing inferior wall ischemia
- Atherosclerotic plaque rupture → platelet aggregation → thrombus formation → complete vessel occlusion
- Myocardial oxygen supply-demand mismatch → ischemia → necrosis within 20-40 minutes
- Troponin and CK-MB release from dying myocytes enabling biochemical diagnosis
C) Immediate Management (8 marks)
- MONA protocol: Morphine (pain relief), Oxygen (if SpO2 <90%), Nitroglycerin (symptom relief), Aspirin 300-325 mg loading dose
- Dual antiplatelet therapy: Aspirin + P2Y12 inhibitor (ticagrelor 180 mg, prasugrel 60 mg, or clopidogrel 600 mg loading)
- Primary PCI within 90 minutes of first medical contact (door-to-balloon time <90 minutes)
- Alternative: Fibrinolytic therapy if PCI unavailable within 120 minutes and symptom duration <12 hours
- Adjunct therapies: Beta-blocker (metoprolol), ACE inhibitor (ramipril), high-intensity statin (atorvastatin 80 mg), anticoagulation (heparin/enoxaparin)
D) Long-Term Secondary Prevention (5 marks)
- Medications: Lifelong aspirin, P2Y12 inhibitor ×12 months minimum, beta-blocker, ACE inhibitor, high-dose statin, consider eplerenone if LVEF ≤40%
- Lifestyle modifications: Smoking cessation, Mediterranean diet, regular exercise 150 min/week, weight management, alcohol limitation
- Cardiac rehabilitation: 12-week supervised program with exercise, education, psychosocial support
- Risk factor control: BP <130/80 mmHg, LDL <70 mg/dL, HbA1c <7% if diabetic
- Follow-up: Regular cardiology review, stress testing at 3-6 months, echocardiography to assess LV function
Question 2: Short Essay Question (10 Marks)
Q: Describe the ECG criteria for STEMI diagnosis and explain how to identify the culprit coronary artery based on ECG lead involvement.
Model Answer (10 Marks Allocation):
A) ST-Elevation Criteria (4 marks)
- General criteria: ST elevation ≥1 mm (0.1 mV) measured at J-point in two anatomically contiguous leads
- Anterior leads (V2-V3) age/gender-adjusted:
- Men <40 years: ≥2.5 mm
- Men ≥40 years: ≥2.0 mm
- Women (any age): ≥1.5 mm
- Contiguous leads definition: Anatomically neighboring leads reflecting same myocardial territory (e.g., V1-V6, II/III/aVF, I/aVL)
- Measurement: J-point elevation assessed 0.04 seconds after QRS complex ends
B) Coronary Artery Localization (6 marks)
Inferior MI (II, III, aVF):
- Right coronary artery (RCA) – 80% of cases
- Left circumflex (LCx) – 20% of cases
- Differentiation: Lead III > Lead II suggests RCA; reciprocal depression in I/aVL confirms diagnosis
Anterior MI (V1-V4):
- Left anterior descending (LAD) artery occlusion
- Extensive anterior (V1-V6, I, aVL): Proximal LAD
- Localized anterior (V2-V4): Mid-LAD
Lateral MI (I, aVL, V5-V6):
- Left circumflex artery or LAD diagonal branches
- High lateral (I, aVL): First diagonal or LCx
- Inferolateral (II, III, aVF + V5-V6): Dominant LCx
Posterior MI:
- ST depression V1-V3 with tall R waves (mirror image)
- True posterior leads V7-V9 show ST elevation
- Usually LCx or RCA posterior descending branch
Question 3: Short Answer Question (5 Marks)
Q: What is the high-sensitivity troponin 0/1-hour algorithm for ruling out acute MI? Include specific cut-off values.
Model Answer:
0/1-Hour Algorithm (5 marks):
Rule-Out Criteria (Safe Discharge):
- hs-cTnT <5 ng/L at presentation (0 hour) AND delta change <3 ng/L at 1 hour
- Negative predictive value >99.5%
- Requires low clinical probability and non-ischemic ECG
Rule-In Criteria (Confirm MI):
- hs-cTnT ≥52 ng/L at presentation OR rise ≥5 ng/L at 1 hour
- Positive predictive value 70-75%
- Requires clinical and ECG correlation
Observation Zone:
- Values between rule-out and rule-in thresholds
- Requires extended observation, repeat testing at 3-6 hours, or alternative testing
- Consider non-ischemic causes of troponin elevation
Viva Tips for Acute Myocardial Infarction Topic
Examiner Favourites:
- Draw and explain the coronary circulation and territories on provided diagram
- Interpret sample ECGs identifying STEMI location and reciprocal changes
- Recite door-to-balloon time targets (90 minutes) and justify urgency
- Calculate GRACE score or TIMI risk score from provided patient data
- List absolute and relative contraindications to fibrinolytic therapy
Clinical Scenario Preparation:
- Be ready to manage simulated MI case from ED presentation through discharge planning
- Know drug dosing precisely (aspirin 300 mg, ticagrelor 180 mg, etc.)
- Understand when to choose PCI vs. fibrinolysis based on time and resources
Last-Minute Checklist
Must-Know Facts:
✓ STEMI criteria: ≥1 mm in limbs, ≥2 mm in V2-V3 (men >40), ≥2.5 mm (men <40), ≥1.5 mm (women)
✓ Aspirin 300 mg + P2Y12 inhibitor loading immediately
✓ Door-to-balloon <90 minutes for primary PCI
✓ DAPT minimum 12 months post-MI
✓ Troponin >99th percentile + clinical ischemia = MI diagnosis
✓ Mediterranean diet + exercise + smoking cessation = 50-60% event reduction
✓ Cardiac rehabilitation reduces mortality 20-30%
Common Exam Traps:
- Don’t confuse STEMI ECG with left ventricular hypertrophy or early repolarization patterns
- Remember gender/age-adjusted criteria for V2-V3 leads
- Know that troponin elevation ≠ always MI (consider myocarditis, PE, renal failure)
- Reciprocal depression increases specificity but isn’t required for diagnosis
Conclusion
Acute Myocardial Infarction (MI) remains a leading cause of mortality globally, with distinct epidemiological patterns affecting both developed nations like the United States and rapidly developing countries like India. Mastering ECG interpretation skills to differentiate STEMI ECG changes from NSTEMI ECG changes, understanding cardiac troponin diagnostic algorithms, and implementing evidence-based immediate management protocols saves lives in critical moments.
The evolution from acute treatment to comprehensive post-MI care plan strategies—including optimized pharmacotherapy, lifestyle changes after heart attack, and structured cardiac rehabilitation after MI programs—determines long-term prognosis and quality of life. With adherence to dual antiplatelet therapy for MI protocols and aggressive secondary prevention measures, mortality rates continue declining even as disease prevalence rises.
Simply MBBS provides evidence-based medical education resources helping students, doctors, and health enthusiasts navigate complex cardiovascular topics. Subscribe to our newsletter at simplymbbs.com for weekly updates on clinical medicine, exam preparation strategies, and the latest research insights. Share this comprehensive guide with colleagues preparing for medical examinations or managing MI patients, and explore our related content on ECG interpretation techniques and heart failure management for deeper cardiovascular knowledge.