Acute barbiturate poisoning is a medical emergency that requires prompt intervention. Barbiturates, once popular for treating anxiety and insomnia, have now been largely replaced by safer alternatives. However, these drugs are still found in various forms and can lead to severe poisoning if misused. Understanding how acute barbiturate poisoning affects the body, its symptoms, and its treatment options is crucial for medical professionals, students, and the general public.
In this article, we will explore the causes, symptoms, diagnosis, treatment, and prevention of acute barbiturate poisoning.
What is Acute Barbiturate Poisoning?
Acute barbiturate poisoning refers to the harmful effects caused by an overdose of barbiturates. Barbiturates are central nervous system depressants that were once commonly prescribed for conditions like anxiety, insomnia, and seizures. When consumed in excessive amounts, barbiturates can cause serious toxicity and potentially life-threatening symptoms.
Barbiturates work by enhancing the activity of GABA (gamma-aminobutyric acid), an inhibitory neurotransmitter, leading to sedation, muscle relaxation, and a slowing down of brain activity. In high doses, they can cause respiratory depression, coma, and even death.
For more information on toxicology in medical practice, visit our Medical Poisoning Guide.
Why It Matters: The Importance of Recognizing Acute Barbiturate Poisoning
Understanding about this poisoning is vital for several reasons:
- Public Health Concern: While the use of barbiturates has declined, they are still present in medical settings, and their misuse continues to pose a risk, particularly in cases of overdose or intentional ingestion.
- Medical Relevance for MBBS Students: Medical students need to familiarize themselves with the symptoms, diagnosis, and treatment protocols associated with barbiturate poisoning as part of their clinical education.
- Real-Life Application: For healthcare providers, timely intervention can save lives. Knowing the symptoms and treatment options can help them deliver appropriate care to patients in distress.
Key Points to Understand Acute Barbiturate Poisoning
- Primary cause: Overdose of barbiturates or accidental ingestion.
- Symptoms: Respiratory depression, coma, hypotension, and confusion.
- Management: Immediate hospitalization, administration of activated charcoal, and supportive treatment.
- Prognosis: Timely intervention can lead to a good recovery, but severe cases may result in death.
Epidemiology and Common Scenarios
- Barbiturate poisoning now comprises a small fraction of all drug overdoses but is still encountered, particularly in attempted suicides or accidental pediatric ingestions.
- Most common among: elderly on long-term prescriptions, individuals with psychiatric disorders, and intentional self-harm cases.
Pharmacology Recap & Pathophysiology
- Mechanism: Barbiturates increase GABAergic neurotransmission, profoundly depressing neuronal firing in the brain and spinal cord.
- Key Point: The margin of safety between a sedative and a lethal dose is very small.
- Toxic Dose: Varies by drug; even 2-3x the normal dose may be fatal, especially with short-acting barbiturates (e.g., pentobarbital, secobarbital).
Causes & Risk Factors
- Intentional Overdose: Most common – suicide attempts.
- Accidental Ingestion: Seen in children, confused elderly, or those on multiple medications.
- Polypharmacy: Combination with alcohol, benzodiazepines, or other CNS depressants increases risk.
- Therapeutic Error: Dosage mistakes or renal/hepatic impairment reducing clearance.
Clinical Features: Stages & Symptoms
Symptoms depend on dose and time since ingestion:
Early Features (within 1–6 hours)
- Drowsiness, disorientation
- Slurred speech, ataxia
- Nystagmus
Moderate to Severe Poisoning
- Stupor or coma
- Hypothermia
- Flaccid muscles (may mimic brain death)
Danger Signs
- Respiratory depression or apnea
- Profound hypotension
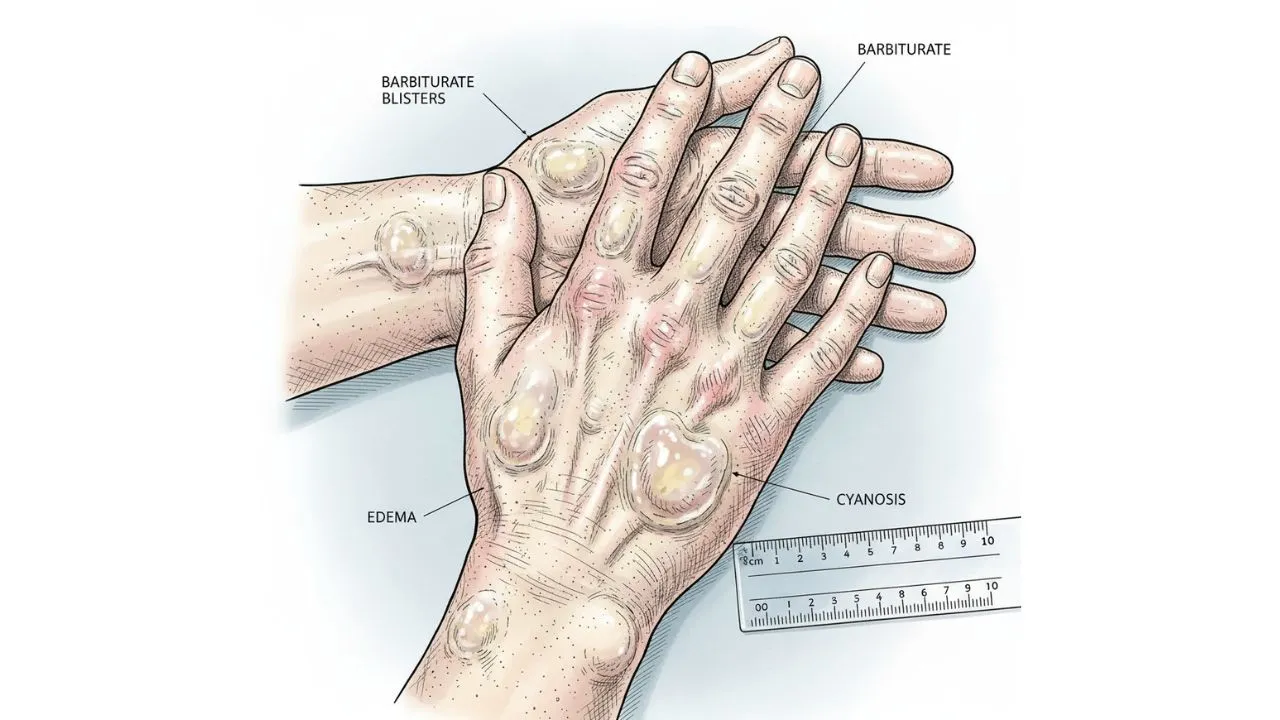
- Bullous skin lesions (“barbiturate blisters”)
Diagnosis: Clinical & Laboratory Approach
1. Clinical Diagnosis
- History of ingestion or empty bottles
- Smell of barbiturates (“medicinal” odor) on breath
- Deep coma with preserved pupillary light reflex (helpful clue)
2. Investigations
- ABG: respiratory acidosis with hypoxemia
- Serum barbiturate level (may not be available fast enough)
- Rule out co-ingestants (paracetamol, alcohol, benzodiazepines)
- Baseline renal, liver function, and electrolytes
Differential Diagnosis
- Benzodiazepine, alcohol, opioid, tricyclic antidepressant, or carbon monoxide toxicity
- Hypoglycemia
Management Protocol: Stepwise Emergency Care
1. Initial stabilization
- Airway: Secure and protect
- Breathing: Assist or intubate if necessary
- Circulation: IV fluids for hypotension, monitor ECG
2. Decontamination
-
Within 1 hour: Administer activated charcoal if airway protected
3. Supportive Care (mainstay)
- Mechanical ventilation if respiratory depression severe
- Warming blankets for hypothermia
- Frequent turning to prevent pressure sores
- Treat infection if aspiration pneumonia occurs
4. Enhanced Elimination
- Urine alkalinization (for phenobarbital only): IV sodium bicarbonate may speed renal excretion
- Hemodialysis: In severe poisoning, especially with phenobarbital
5. Antidote
-
No specific antidote exists
6. Monitoring & Disposition
-
Continuous cardiac, respiratory, and neurological monitoring in ICU for severe cases
Complications & Prognosis
- Complications: Pneumonia, sepsis, rhabdomyolysis, renal failure, aspiration, skin necrosis
- Mortality: Decreases significantly with rapid hospital care; delayed intervention may result in death (mainly due to apnea or circulatory collapse)
Prevention & Patient Education
- Use safer alternatives (benzodiazepines) for sleep/anxiety when indicated
- Safe medication storage, especially around children and the elderly
- Educate mental health patients on medication safety; limit dispensing to small quantities when at risk
Case Study Example
Case: A 35-year-old male is found unconscious with shallow breathing after ingesting 30 unknown tablets. On arrival: unresponsive, BP 80/60 mmHg, RR 6/min, pupils sluggish but reactive, T 34°C. Labs: respiratory acidosis.
Approach: Immediate airway support, activated charcoal, warming, ICU admit. Patient required ventilation for 48 hours, then gradually regained consciousness and fully recovered by day 4.
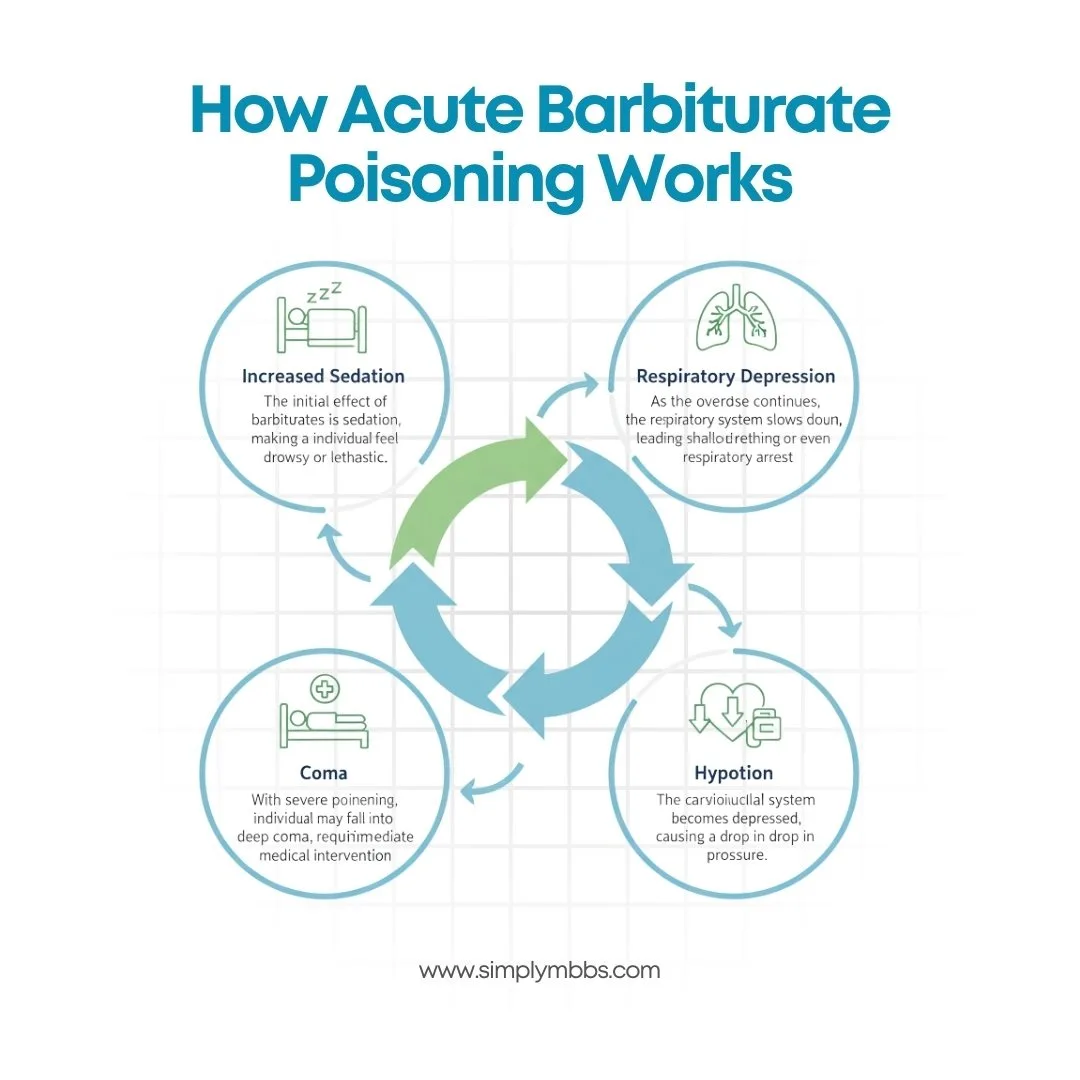
How Acute Barbiturate Poisoning Works
The pathophysiology of this poisoning involves the inhibition of the central nervous system (CNS). Barbiturates bind to the GABA-A receptor, enhancing the effects of GABA, which in turn suppresses neuronal excitability. This leads to a sedative effect, but when the dose exceeds the therapeutic range, it can cause significant CNS depression.
Here’s how the body responds to an overdose:
- Increased Sedation: The initial effect of barbiturates is sedation, making the individual feel drowsy or lethargic.
- Respiratory Depression: As the overdose continues, the respiratory system slows down, leading to shallow breathing or even respiratory arrest.
- Hypotension: The cardiovascular system becomes depressed, causing a drop in blood pressure.
- Coma: With severe poisoning, the individual may fall into a deep coma, requiring immediate medical intervention.
Comparison: Barbiturate Poisoning vs Other Types of Poisoning
It’s important to understand how the poisoning compares with other types of poisoning, such as opioid or benzodiazepine poisoning. Here’s a brief comparison:
| Feature | Barbiturate Poisoning | Opioid Poisoning | Benzodiazepine Poisoning |
|---|---|---|---|
| Mechanism | CNS depression, GABA enhancement | CNS depression, mu-opioid receptor binding | CNS depression, GABA enhancement |
| Symptoms | Respiratory depression, coma, hypotension | Respiratory depression, pinpoint pupils, bradycardia | Sedation, confusion, dizziness |
| Treatment | Activated charcoal, supportive care | Naloxone, supportive care | Flumazenil (rarely used), supportive care |
| Prognosis | Depends on the dose and timing of treatment | High recovery rate with timely intervention | Good prognosis with proper care |
While both barbiturate and opioid poisoning can lead to life-threatening symptoms like respiratory depression, their treatments differ significantly. Barbiturates require prompt supportive care, while opioids can often be reversed with naloxone.
Expert Insights / Data-Driven Points
- According to a study published in The American Journal of Emergency Medicine, barbiturate overdoses contribute to a significant number of poisoning cases in emergency rooms, with a mortality rate of 5-10% in untreated severe cases.
- The U.S. Poison Control Centers report an increase in barbiturate poisoning, particularly among older adults who may have been prescribed these drugs in the past and are unaware of the dangers of overdose.
Common Mistakes to Avoid in Acute Barbiturate Poisoning Management
- Delayed Diagnosis: It’s essential to recognize the symptoms of acute barbiturate poisoning early to initiate treatment promptly.
- Incorrect Treatment: Administering inappropriate treatments, such as narcotics for respiratory depression, can worsen the condition.
- Ignoring Supportive Care: Supportive care, including mechanical ventilation, is crucial in managing severe poisoning cases.
- Failure to Monitor: Continuous monitoring of vital signs (respiration, blood pressure) is vital to prevent complications.
Frequently Asked Questions (FAQs)
Q. What is acute barbiturate poisoning?
A : Acute barbiturate poisoning occurs when someone ingests an overdose of barbiturates, leading to severe central nervous system depression, respiratory issues, and potential death.
Q. How does acute barbiturate poisoning kill the body?
A : The primary cause of death in acute barbiturate poisoning is respiratory depression. As the overdose progresses, the individual may stop breathing, leading to hypoxia and multi-organ failure.
Q. What are the symptoms of acute barbiturate poisoning?
A : Common symptoms include confusion, dizziness, respiratory depression, hypotension, and, in severe cases, coma and death.
Q. How is acute barbiturate poisoning treated?
A : Treatment involves hospitalization, activated charcoal administration (if the poisoning occurred recently), and respiratory support (such as mechanical ventilation) in severe cases.
Exam Question–Answer (University Pattern)
Q: Define acute barbiturate poisoning and explain its management.
Answer:
- Definition: Acute barbiturate poisoning occurs due to an overdose of barbiturates, leading to central nervous system depression and respiratory failure.
- Symptoms: Respiratory depression, confusion, hypotension, coma.
- Management:
- Initial assessment: Ensure airway protection, assess vitals.
- Activated Charcoal: Administer if within 1 hour of ingestion.
- Supportive Care: Mechanical ventilation, IV fluids.
- Monitoring: Continuous vital sign monitoring.
Marks Distribution:
- Definition: 2 marks
- Symptoms: 3 marks
- Management: 5 marks
Answer:
Acute barbiturate poisoning is a life-threatening condition resulting from the ingestion or administration of excessive doses of barbiturate drugs, leading to profound central nervous system (CNS) depression, respiratory compromise, and cardiovascular instability. Early recognition and prompt, systematic management are crucial to prevent morbidity and mortality.
Definition (2 Marks)
Acute barbiturate poisoning occurs when plasma concentrations of barbiturates exceed the therapeutic range, causing excessive CNS depression. Barbiturates enhance γ-aminobutyric acid (GABA)–mediated inhibition in the brain, resulting in sedation, hypnosis, and, at toxic levels, coma and respiratory arrest.
Pathophysiology
Barbiturates increase the duration of chloride channel opening at the GABA_A receptor, amplifying inhibitory neurotransmission. At high doses, they depress neuronal activity in the brainstem respiratory center, impairing respiratory drive and leading to hypoventilation, hypoxia, and hypercapnia. Cardiovascular depression occurs via direct myocardial depression and vasodilation.
Clinical Features (3 Marks)
The severity of presentation correlates with the ingested dose:
-
Mild to Moderate Toxicity
- Drowsiness, ataxia, slurred speech
- Confusion, diminished reflexes
- Nystagmus
-
Severe Toxicity
- Deep coma, unresponsiveness
- Marked respiratory depression (respiratory rate <8 breaths/min)
- Hypotension (systolic blood pressure <90 mmHg)
- Hypothermia, bradycardia
-
Life-Threatening Signs
- Apnea and respiratory arrest
- Cardiovascular collapse
- Fixed, dilated pupils
Diagnosis
- History and Examination: Confirm barbiturate use or overdose; assess vital signs and neurological status.
- Laboratory Tests: Serum barbiturate levels (if available), arterial blood gas analysis (to detect respiratory acidosis), electrolytes, renal and liver function tests.
- Electrocardiogram: To evaluate for arrhythmias and conduction abnormalities.
Management (5 Marks)
1. Initial Assessment and Stabilization
- Airway Protection: Assess and secure airway; consider endotracheal intubation if Glasgow Coma Scale ≤8 or if airway reflexes are compromised.
- Breathing: Provide supplemental oxygen and assist ventilation; initiate mechanical ventilation for persistent hypoventilation or apnea.
- Circulation: Establish intravenous access; monitor heart rate, blood pressure, and oxygen saturation continuously. Administer intravenous crystalloids to maintain adequate perfusion.
2. Decontamination
- Activated Charcoal: Administer a single dose (1 g/kg, up to 50 g) if the patient presents within 1 hour of ingestion, and the airway is protected or patient is alert enough to swallow safely.
- Gastric Lavage: Consider only within 1 hour of a large, life-threatening ingestion and if performed by experienced personnel with airway protection in place.
3. Enhanced Elimination
- Alkaline Diuresis: Not routinely recommended as barbiturates are weak acids; may be considered for phenobarbital poisoning under strict monitoring of pH and electrolytes.
- Hemodialysis: Indicated for severe phenobarbital overdose, refractory hypotension, prolonged coma, or when serum levels remain elevated despite supportive care.
4. Supportive Care
- Ventilatory Support: Continue mechanical ventilation until the patient regains adequate spontaneous respiratory drive and protective reflexes.
- Cardiovascular Support: Use vasopressors (e.g., norepinephrine) for persistent hypotension despite fluid resuscitation.
- Temperature Management: Maintain normothermia with external warming if hypothermic.
- Monitoring: Hourly neurological checks, continuous cardiac monitoring, frequent arterial blood gas and electrolyte assessments.
5. Observation and Disposition
- Admit to an intensive care unit for severe cases.
- Observe milder cases in a high-dependency unit until CNS depression resolves and vital signs stabilize.
- Psychiatric evaluation prior to discharge in cases of intentional overdose.
Prognosis
With prompt, appropriate treatment, most patients recover fully. Prolonged respiratory arrest or cardiovascular collapse can lead to hypoxic brain injury and increased mortality risk.
Conclusion
This poisoning is a serious medical emergency that requires prompt recognition and treatment. By understanding the symptoms, causes, and treatment options, medical professionals, MBBS students, and the general public can better manage and prevent the consequences of barbiturate overdoses. Remember, the earlier the intervention, the better the chances of a positive outcome.
Stay informed by subscribing to our newsletter for more health tips, medical insights, and educational resources on toxicology and medical emergencies.