Introduction
HIV and AIDS can feel complex, yet the essentials are simple and hopeful. With early testing and modern treatment, people live long, healthy lives. Moreover, prevention works. In this guide, you will learn what HIV and AIDS mean, how HIV spreads, and which symptoms may appear. You will also learn the testing timeline, the window period, and why U=U (undetectable equals untransmittable) matters.
Next, we explain antiretroviral therapy (ART) in plain words. We outline side effects, routine monitoring, and long-acting options where available. Then we give practical prevention steps, including PrEP before exposure and PEP after exposure. Finally, for students, we include exam-style stems, model answers, a diagram prompt, viva one-liners, and a last-minute checklist. (Educational only.)
What is HIV and AIDS?
HIV (human immunodeficiency virus) attacks CD4 T-cells, which coordinate immune defense. AIDS (acquired immunodeficiency syndrome) is the most advanced stage, diagnosed by very low CD4 counts or specific serious infections and cancers. However, with effective ART, most people never reach AIDS and can live long lives. When treatment drives the viral load to “undetectable,” sexual transmission does not occur—U=U.
Quick takeaway: HIV is manageable. Testing and treatment protect health and prevent spread. CDC
How HIV Spreads (HIV transmission)
Common routes
- Vaginal or anal sex without condoms or without effective treatment.
- Sharing needles or syringes.
- Mother-to-child during pregnancy, birth, or breastfeeding without preventive care.
- Blood transfusion in settings without strict screening.
Not transmitted by…
Hugging, handshakes, toilets, casual kissing, sharing dishes, sweat, tears, or mosquito bites. Daily contact is safe. CDC
Why this matters: Understanding true routes reduces fear and fights stigma.
Recognising HIV: Early and Late Features (HIV symptoms, AIDS stages)
Many people have no symptoms for years. Testing is the only way to know.
Table 1. Features across phases
| Phase | Typical timeframe | Key features | Notes |
|---|---|---|---|
| Acute HIV infection | 2–6 weeks after exposure | Fever, sore throat, rash, swollen nodes | Flu-like; resolves on its own |
| Chronic infection | Months–years | Often asymptomatic; mild recurrent infections | Regular care maintains health |
| Advanced disease (AIDS) | Variable | Opportunistic infections (OIs), weight loss, night sweats | Defined by CD4 criteria or AIDS-defining illnesses |
Exam tip: Symptoms alone never confirm or exclude HIV; the algorithm depends on tests and timing. HIVinfo
Testing & Diagnosis: From Window Period to Viral Load
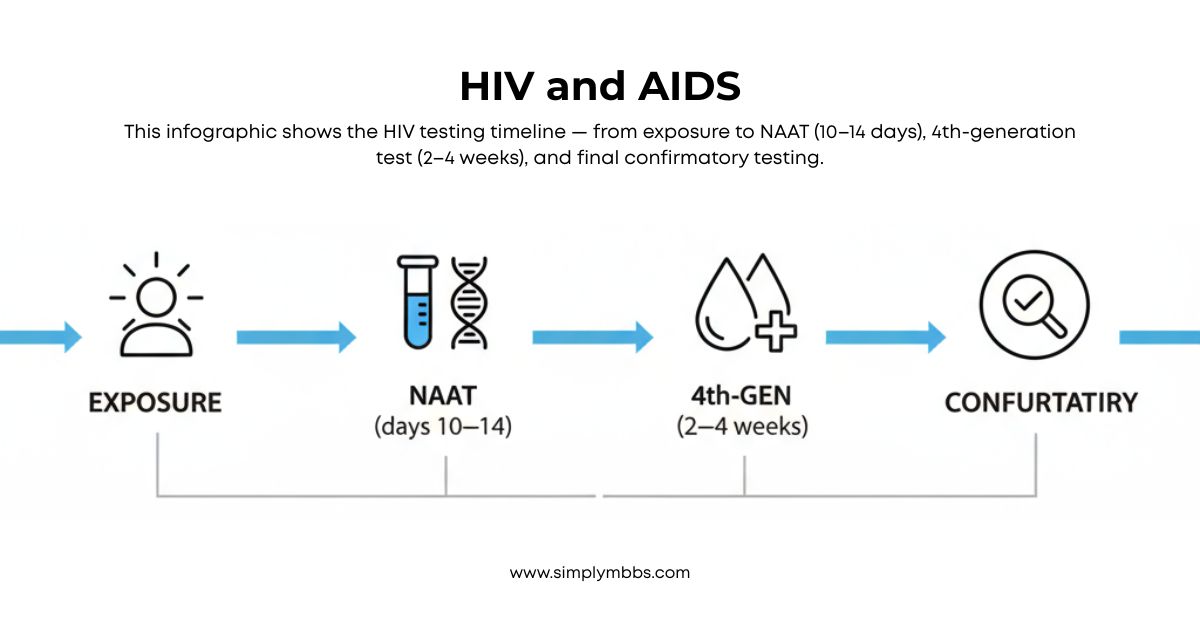
Window period = time between exposure and when a test turns positive. Modern 4th-generation antigen/antibody tests detect most infections by 2–4 weeks. NAAT (nucleic acid amplification) detects even earlier. After a reactive screening test, labs use confirmatory assays. CDC
- CD4 count shows immune strength.
- Viral load shows virus levels; the goal is undetectable.
- Self-tests exist in many countries; confirm positive or unclear results in a clinic.
- Routine testing: Everyone 13–64 years should test at least once; higher-risk groups test more often.
- Table 2. Typical detection windows
| Test | What it detects | Earliest reliable detection (approx.) |
|---|---|---|
| NAAT (RNA/DNA) | Viral genetic material | ~10–14 days after exposure |
| 4th-gen Ag/Ab | p24 antigen + antibodies | ~2–4 weeks after exposure |
| 3rd-gen Ab | Antibodies only | ~3–8 weeks after exposure |
Treatment Overview: ART in Plain Words (antiretroviral therapy, ART)
ART is a combination of medicines that stop HIV from multiplying. As a result, CD4 cells recover, illnesses decline, and life expectancy improves. Today, most people reach undetectable levels within months and maintain them with good adherence. In some settings, long-acting injectables are available under specialist care. HIVinfo
Goals: U=U and adherence
- U=U: An undetectable viral load means no sexual transmission.
- Restore and preserve immune function.
- Prevent opportunistic infections and HIV-related conditions.
Monitoring and safety
- Viral load every few months; CD4 as advised.
- Discuss drug interactions, pregnancy plans, mental health, and travel.
- Do not stop medicines without medical advice.
Prevention You Can Use Today (HIV prevention, PrEP, PEP)
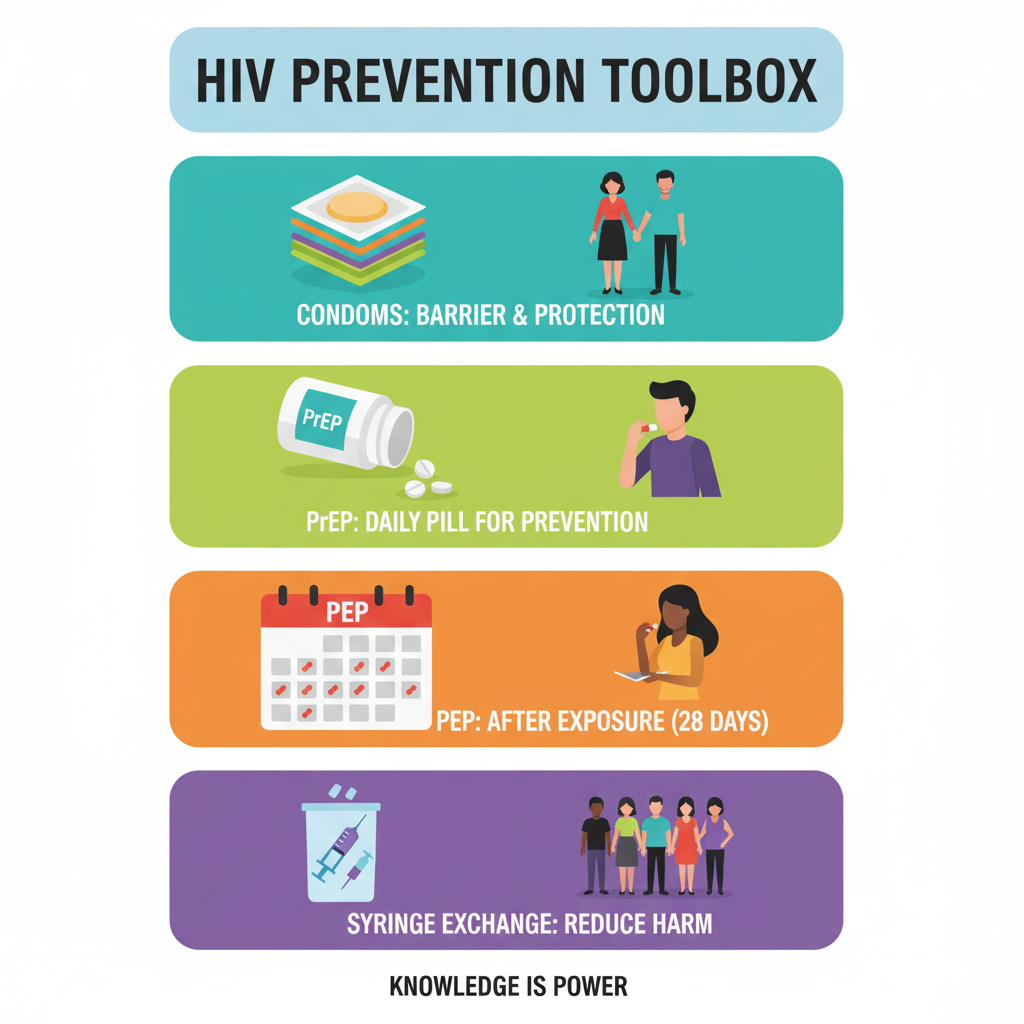
- Condoms: Use correctly and consistently.
- PrEP (pre-exposure prophylaxis): Medicine taken before exposure that greatly reduces risk from sex or injecting.
- PEP (post-exposure prophylaxis): A 28-day course started within 72 hours after a high-risk exposure.
- Never share needles; use sterile equipment and needle-exchange services where available.
- Regular testing and partner care: When a partner with HIV is undetectable, sexual transmission does not occur.
(Follow national guidance for exact regimens and eligibility.)
Clinical Relevance for Students
At-a-glance OIs and common CD4 thresholds
| Opportunistic infection | Usual CD4 (cells/µL) | Key clues | Typical preventive/Tx notes* |
|---|---|---|---|
| PCP (P. jirovecii) | <200 | Dry cough, dyspnea, hypoxemia | TMP-SMX; steroids if severe |
| Toxoplasmosis | <100 | Headache, focal deficits | TMP-SMX prophylaxis when indicated |
| CMV retinitis | <50 | Floaters, visual loss | Urgent ophthalmology; antivirals |
| Oropharyngeal candidiasis | Any, common <200 | Oral plaques, dysphagia | Topical/systemic azoles |
| Tuberculosis | Any | Fever, cough, weight loss | Programmatic TB care |
*Always follow local and national guidelines. (Overview aligns with standard NIH/CDC tables.) HIVinfo
Counseling & infection control
- Use stigma-free language and protect confidentiality.
- Encourage partner testing and PrEP/PEP discussions when relevant.
- Follow needle-stick protocols and standard precautions.
Prevention & Care: Practical Tips
- Keep all clinic appointments and set reminders.
- Ask about vaccines (e.g., hepatitis B, influenza, pneumococcal).
- Maintain nutrition, sleep, and mental health support.
- Discuss pregnancy planning and infant-feeding advice early.
- Join supportive communities if available.
Internal Study Boosters
- Build lymphatic logic with the thoracic duct clinicals. Simply MBBS
- Revise venous routes via azygos vein anatomy. Simply MBBS
- Refresh limb movements using shoulder joint exam notes. Simply MBBS
- Anchor peritoneal spaces with lesser sac overview. Simply MBBS
- Link immunity basics with plasma proteins explained. Simply MBBS
- (Use these for spaced revision and anchor concepts.)
Exam Question–Answer (University Pattern)
Exam stem (verbatim):
“Describe HIV and AIDS under (a) Definition and virology (b) Modes of transmission (c) Clinical features and diagnosis (d) Applied/Clinical aspects including prevention and treatment.”
Suggested marks (Total 10): (a) 2 | (b) 2 | (c) 3 | (d) 3
Model answer :
(a) Definition and virology (2):
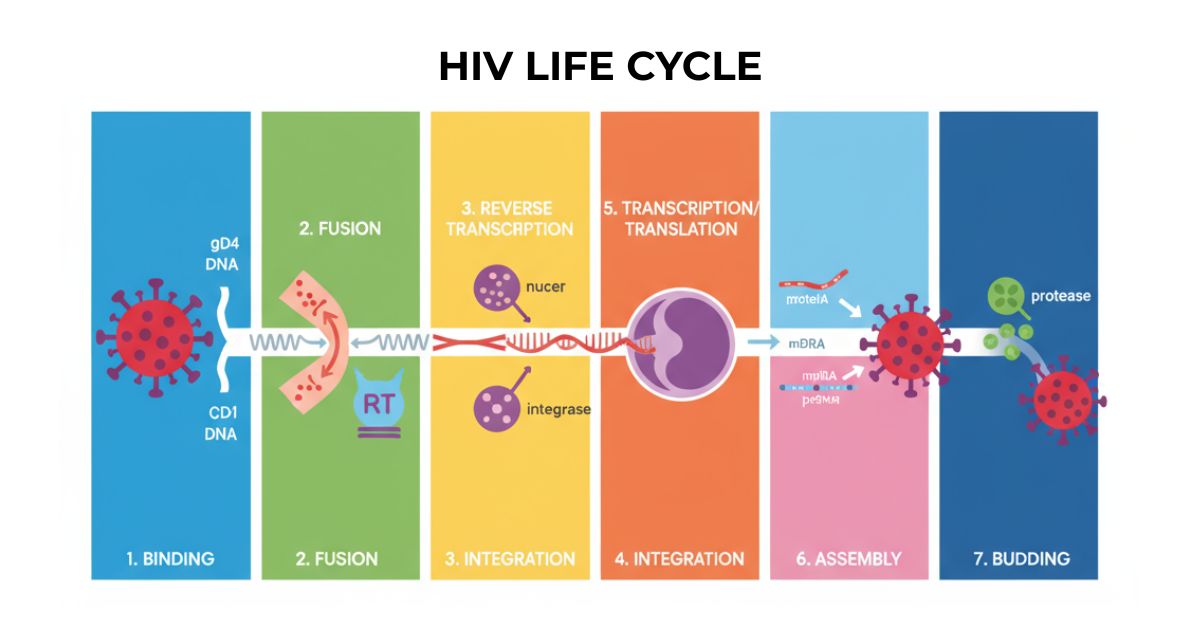
- HIV: retrovirus infecting CD4 T-cells; types HIV-1 and HIV-2.
- Entry via gp120/gp41; enzymes reverse transcriptase, integrase, protease; lifelong infection.
(b) Modes of transmission (2):
- Unprotected vaginal/anal sex; higher risk with high viral load.
- Blood exposure: needles, unscreened transfusions, occupational injuries.
- Mother-to-child during pregnancy, delivery, breastfeeding without prophylaxis. CDC
(c) Clinical features and diagnosis (3):
- Acute phase: fever, rash, pharyngitis, lymphadenopathy.
- Chronic phase: asymptomatic or mild illness for years.
- AIDS: OIs and cancers; defined by CD4 or illnesses.
- Diagnosis: 4th-gen Ag/Ab, confirmatory testing; NAAT early.
- Monitoring: viral load and CD4. HIVinfo+1
(d) Applied/Clinical aspects (3):
- ART for all; start promptly; achieve U=U to prevent sexual transmission.
- Prevention: condoms, PrEP, PEP <72 hours, harm reduction.
- OIs prophylaxis by CD4 thresholds; immunizations; adherence counseling.
Simple diagram prompt (one line):
“Sketch HIV virion: envelope with gp120/gp41 spikes; matrix; conical capsid; RNA; reverse transcriptase; label entry and replication steps.”
Viva quick hits (one-liners):
- What is U=U? Undetectable viral load means no sexual transmission.
- Window period? Time before tests detect infection.
- First-line screening test? 4th-gen antigen/antibody combo.
- When to start ART? As soon as diagnosed.
- PEP window? Start within 72 hours; continue 28 days.
- PrEP vs PEP? PrEP before risk; PEP after risk.
- CD4 for PCP risk? Usually <200 cells/µL.
- Why adherence? Prevents failure and resistance.
Last-minute checklist (5–7 bullets):
- Define HIV vs AIDS; state U=U.
- Real routes vs myths.
- Tests: 4th-gen, NAAT, window timing.
- ART goals; monitoring plan.
- PrEP/PEP timings.
- OIs table with CD4 cut-offs.
FAQs (patient-friendly)
-
What is the difference between HIV and AIDS?
HIV is the virus. AIDS is the late stage when the immune system is very weak. -
How soon can I test after a risk?
Most 4th-generation tests detect infection by 2–4 weeks. Repeat if tested early. Confirm results with a clinician. -
Can treatment stop transmission?
Yes. When the viral load stays undetectable, sexual transmission does not occur (U=U). -
What is PrEP?
PrEP is medicine taken before exposure to reduce risk from sex or injecting. It works best with regular use. -
What is PEP?
PEP is a 28-day course started within 72 hours after a high-risk exposure. Seek care immediately. -
Do mosquitoes spread HIV?
No. HIV does not spread through mosquitoes, hugging, or casual contact. -
Should I stop breastfeeding if I have HIV?
Follow local clinical guidance. Teams individualize advice to minimise infant risk.
Conclusion
You now have a clear view of HIV and AIDS—how it spreads, how testing works, and how ART turns HIV into a manageable condition while ensuring U=U. Keep learning with our focused explainers: thoracic duct, azygos vein, shoulder joint, lesser sac, and plasma proteins for exam-ready integration. If you have personal concerns, please speak with a qualified clinician.