Iron poisoning is a life-threatening medical emergency, especially in children and young adults. Understanding iron toxicity stages, clinical features, and rapid management of these iron poisoning cases is crucial for exam success and effective real-world care. This complete iron poisoning guide covers all you need – definition, causes, pathophysiology, symptoms, treatment, prevention, practical checklists, and MBBS-focused FAQs.
What is Iron Poisoning?
Iron poisoning is acute systemic toxicity caused by the ingestion of a toxic dose of iron. Most cases result from overdose of iron tablets or syrup, usually in children. Severe iron toxicity rapidly leads to multi-organ failure, making early recognition and treatment vital.
- Common sources: Adult-strength iron tablets, pediatric multivitamin-iron syrups/tablets, prenatal supplements.
- Key demographic: Children under 5 years (NCBI StatPearls)
Iron Toxicity Pathophysiology
Iron is a potent cellular toxin in overdose. It catalyzes free radical formation, directly injures the gastrointestinal mucosa, and overwhelms protein-binding leading to metabolic acidosis, shock, and organ dysfunction in iron toxicity cases.
- Initial insult: Corrosive injury to GI tract, vomiting/hemorrhage
- Systemic effects: Mitochondrial dysfunction, hepatotoxicity, coagulopathy
- Stages progress rapidly. Early intervention is critical!
Clinical Stages of Iron Toxicity
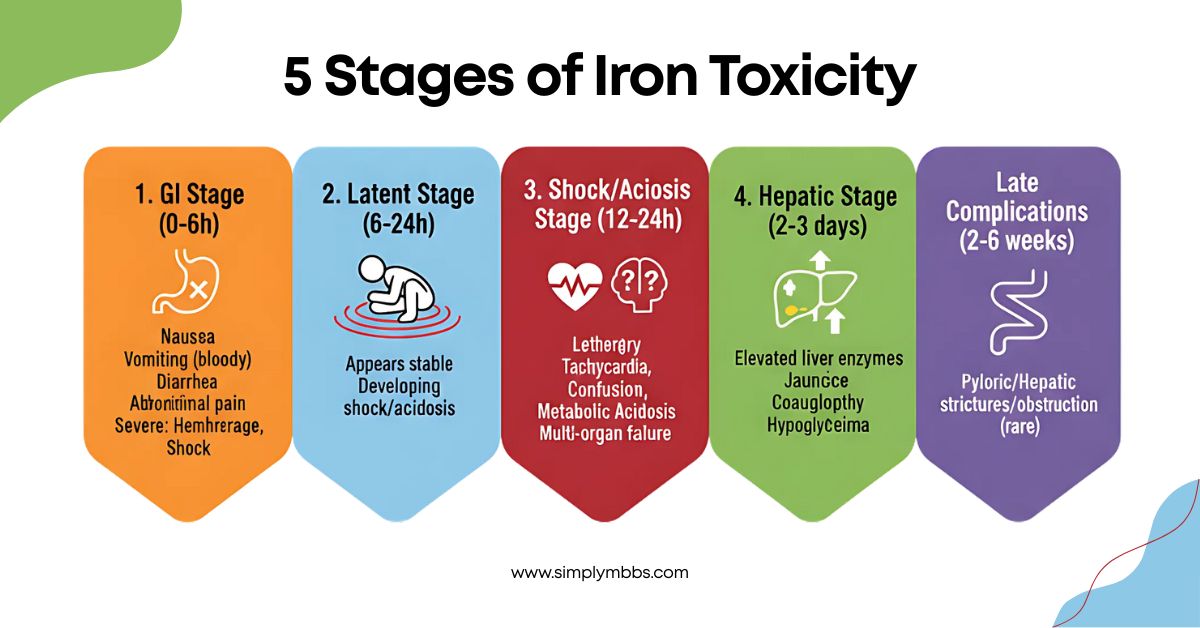
Recognizing the five stages of iron toxicity is essential for proper management:
- 1. GI Stage (0-6h): Nausea, vomiting (may be bloody), diarrhea, abdominal pain. Severe cases: GI hemorrhage, shock.
- 2. Latent Stage (6-24h): Patient may appear stable, but shock/metabolic acidosis are developing.
- 3. Shock/Acidosis Stage (12-24h): Lethargy, tachycardia, hypotension, confusion, metabolic acidosis, multi-organ failure.
- 4. Hepatic Stage (2-3 days): Elevated liver enzymes, jaundice, coagulopathy, hypoglycemia.
- 5. Late Complications (2-6 weeks): Pyloric or hepatic strictures/obstruction (rare).
Diagnosis of Iron Toxicity
Diagnosing iron toxicity requires a comprehensive approach combining history, clinical presentation, and laboratory findings:
- History: Suspect iron toxicity in any child with GI symptoms and access to iron-containing medications.
- X-ray: Many iron tablets are radiopaque – abdominal x-ray can help estimate ingestion.
- Labs: Serum iron (peak 4-6 hours post-ingestion, >350 mcg/dL is significant), anion gap metabolic acidosis, LFTs, renal profile, clotting studies.
Tip: If severe iron toxicity is suspected, treat without waiting for levels!
Iron Poisoning Treatment and Management
Immediate action saves lives in iron poisoning cases! Here’s what to do:
- Decontamination: Whole Bowel Irrigation (WBI) with PEG may be needed for large ingestions (especially if tablets visible on X-ray); gastric lavage if very recent (within 1 hour), but is rarely used.
- Supportive Care: IV fluids, airway protection, monitor glucose/electrolytes, correct shock/acidosis.
- Chelation Therapy: Deferoxamine is the antidote of choice. Indicated for severe iron toxicity, shock, persistent GI symptoms, high iron level or anion gap acidosis. Dose: 15 mg/kg/hr IV; continue until clinical improvement and urine is no longer “rose-pink.” Watch for hypotension and acute lung injury (rare side effect).
- ICU Admission: For severe cases with shock, organ failure, or multi-organ monitoring needs.
For full protocols, see official guidelines at MSD Manual – Iron Poisoning.
Prevention and Public Health in Iron Toxicity
Preventing iron toxicity is crucial for child safety:
- Keep all iron-containing medications far out of reach of children – child-resistant containers are a must!
- Educate caregivers and parents on the dangers of iron supplements, especially prenatal tablets.
- Regulate packaging: single-dose childproof blister packs are recommended.
Also read:Podophyllin poisoning, Methanol poisoning, Anaphylactic shock, Subdural hemorrhage, Hypovolemic shock
Last-Minute MBBS Checklist: Iron Poisoning
Essential points for iron poisoning recognition and management:
- GI+Metabolic acidosis after ingestion = suspect iron poisoning.
- Key Stages: GI upset→ latent → shock → hepatic failure → late stricture
- Labs: Serum iron (>350 mcg/dL), metabolic acidosis, deranged LFTs
- Treatment: Deferoxamine, critical care support, WBI/fluids
- Always prevent access to iron medications in households with children
Model Q&A: University/Exam Prep on Iron Toxicity
Q1. Enumerate the five clinical stages of iron poisoning and their features.
A:
- GI stage: Nausea, vomiting, diarrhea, abdominal pain, GI bleed (0–6h)
- Latent: Apparent recovery, metabolic acidosis developing (6–24h)
- Shock/metabolic: Lethargy, shock, acidosis, organ failure (12–24h)
- Hepatic: Liver failure, coagulopathy, hypoglycemia (2–3d)
- Late complications: Pyloric/stricture, hepatic scarring (2–6wks)
Q2. How is the diagnosis of iron poisoning confirmed in the emergency room?
A: By exposure history, GI symptoms, serum iron >350 mcg/dL (drawn 4–6h post-ingestion), X-ray (radiopaque tablets), acidosis, deranged LFTs.
Q3. What is the antidote for severe iron toxicity?
A: Deferoxamine – an iron chelator given IV (15mg/kg/h) for clinical toxicity, metabolic acidosis, or high serum iron.
Q4. List two major points in the prevention of accidental iron toxicity.
A: Keep iron out of child’s reach, use childproof packaging, and educate caregivers.
Q5. Name a late GI complication of iron toxicity.
A: Pyloric stenosis/stricture.
Conclusion & High-Yield Learning Points on Iron Poisoning
Key takeaways for iron poisoning management:
- Think iron poisoning for any child with sudden GI distress and access to pills!
- Clinical stages progress quickly; early management saves lives in iron toxicity cases.
- Deferoxamine is the essential antidote for severe toxicity.
- Prevention and caregiver education are critical public health measures.
Stay tuned to SimplyMBBS for more high-yield toxicology and clinical guides. Keep learning and keep growing!